ABSTRACT
Background
Geriatric populations have at high probability of getting drug-related issues due to age-related pharmacokinetic and pharmacodynamic changes. Ageing populations are more prone to have DRPs due to age, drug characteristics, polypharmacy, and multiple comorbidities. The study aimed to assess the DRP in geriatric patients attended a tertiary care teaching hospital.
Materials and Methods
The study was a prospective observational study which was carried out for a duration of 6 months involving inpatients of Vivekananda General Hospital. PCNE classification V 9.1 was used to assess the drug-related problems.
Results
In this study, 210 geriatric patients were analysed, among which 161 were males and 49 were females. The mean age of study participants was 69.5 (±5.0) years. Among overall population, 193 (91.9%) subjects were reported with comorbidities. The most common chronic disease was hypertension (43.4%), and the least was found to be Hypothyroidism (1.6%). Comorbidities were assessed based on charlson comorbidity index, where the mean score of comorbidities was 3.86 with 54% survival rate in 10 years. The subjects were analysed for DRPs using PCNE classification V9.1, among which 132 prescriptions contain 299 DRPs. Drug-drug interactions were the highest observed DRPs (107). Other DRPs were found within the Problem domain (23.07%), Cause domain (43.47%), planned interventions (16.72%), Intervention acceptance (11.70%) followed by Outcome domain (5.01%) of PCNE classification.
Conclusion
Our study highlights that importance of pharmaceutical care among the geriatric patients. Special emphasized care must be given to elderly population to avoid DRPs due to presence of comorbidities, polypharmacy and illiteracy.
INTRODUCTION
Elderly populations are at increased risk of Drug-Related Problems (DRPs) because of age-related Pharmacokinetic and Pharmacodynamic (PK-PD) alterations.1,2 The number of older people is projected to grow to about 324 million by 2050, due to advances in medical technology and its significant impact on society, finances and health planning.3 A numerous factor, such as multidrug use concerned with multiple diseases, physiological changes associated with age and changes in PK-PD parameters. Studies of hospitalized elderly patients all over the world have found that DRPs in post-hospital prescribing such as prescribing drugs, administering the prescribed drugs, while dispensing the drug to a patient are common in this susceptible population, including unintended drug discrepancies and Potentially Inappropriate Prescriptions (PIPs).4–6
Population ageing is a natural phenomenon. Over time, the size and proportion of the population of older people is increasing in all countries of the world. Population ageing is an unavoidable demographic reality that accompanies advancements in health and healthcare systems. According to the report of the Expert Committee on Population Projections for India and States 2011-2036, an increase of almost 34 million senior people was noticed in 2021 over the Population Census 2011, and an increase of over 56 million elderly people is projected in 2031. India has earned the tag of “Aging Nation” as 7.75% of the country’s population is over the age of 60 and 75% of the elderly live in rural areas. A report by the ICMR on the chronic disease profile in the geriatric indicated that the most prevalent diseases were anaemia, followed by dental problems, hypertension, COPD, cataracts, and osteoarthritis.4,7
Senescence is related with elevated incidence of many dreadful diseases that lead to an increase in the use of multiple drugs and complicated therapies. Age-associated changes in PK-PD make elderly patients more prone to the drug and more exposed to adverse effects of drug. The greater number of drugs intake leads to higher chances of interactions. The DRP is described as adverse patient events related to therapeutic treatment that are likely to affect the desired patient outcome. The overall goal of drug review is to improve the quality and safety of pharmaceutical treatment.8
These DRPs are concerned with adverse outcomes, such as prolonged hospital stays, deteriorating clinical status, and increased medical costs. Therefore, the treatment of hospitalized geriatric patients demands special care and observation to optimize the drug use quality and reduce or prevent DRPs.9
Prescribing of drugs that show more harm than benefit, especially when safer alternatives exist: prescribing of inappropriate dose or duration of drugs; under-prescribing of potentially beneficial medications; important drug-drug as well as Drug-Disease Interactions (DDIs); and duplication of drugs.10
The DDIs are those with narrow therapeutic indices, those that induce/inhibit microsomal enzymes, those that follow zero-order elimination kinetics, and those that are critical in critically ill patients. It can occur in the presence of elderly patients with kidney/liver impairment and multiple medications. Therapeutic regimen is a major unit of patient care, where utilization of more medications may require treating either a disease or comorbidities, and adverse interactions can occur between these drugs.11
The clinical pharmacist plays an important role in identification, rectifying and preventing DRPs in hospital setup by employing various classification systems such as Pharmaceutical Care Network Europe (PCNE) and American Society of Hospital Pharmacists (ASHP) classification system that helps in management of DRPs.5
The identification, study, categorisation, management and prevention of causes of DRPs are fundamental and integral part of pharmaceutical care services which helps in reducing the occurrence of DRPs in geriatric patients. Many Studies showed that most DRPs are probable and preventable. Pharmacist involvement can reliably enhance patient outcomes, involving medication adherence, pharmacotherapy adequacy, HRQOL, financial status and patient satisfaction, hence we conducted assessment of drug-related problems in the geriatric patients attended a tertiary care teaching hospital.12–14
MATERIALS AND METHODS
The study was a prospective observational study which was carried out for duration of 6 months involving inpatients of Vivekananda General Hospital. Ethical clearance for this study was obtained from the Institutional Ethical Committee (KLECOPH/IEC/2022-23/04).
Inclusion Criteria
Both male and female patients were above the age of 60 and admitted to the hospital more than 48 hr.
Exclusion criteria
Outpatients and patients below the age of 60 years and patients not willing to participate in the study.
Sample size
The total sample size was 210.
Data collection
Data was collected using various sources which involve patient case records, laboratory reports, patient medication chart, clinical progress chart, nurse chart, interaction with the patient, interaction with patient’s caregiver, interaction with healthcare professionals. The study procedure involved the use of various data collection forms for documentation of the data. Patient profile forms, ADR reporting forms, Drug interactions, Clinical pharmacist intervention Reporting forms, Medication history intervention forms, Patient counselling forms, Drug information request, and Documentation forms were used in the study.
PCNE classification V.9.1 was used to assess DRPs, while IBM Micromedex was used to determine drug-drug interactions. Comorbidities were assessed using charlson comorbidity index. Excel database was used to assess and store the data collected throughout study. Descriptive statistics where categorical variables are expressed in terms of frequencies and percentage. Continuous variables are presented using mean and standard deviation. Pivot analysis was used for extracting the data for observational analysis, organizing and data structuring.
RESULTS
Demographics and baseline characteristics of study population
Total of 210 elderly subjects were enrolled in the study. Among these, 161 (76.6%) were males and 49 (23.3%) were females. The mean age of study participants was 69.5 (±5.0) years. Majority of participants 116 (55.2%) were found within the age group of 60-69 years. The study also analysed the literacy rate wherein 72 (34.3%) were literate and 138 (65.7%) were illiterate or did not have a formal education. Majority of them were residing in rural areas 130 (61.9%), whereas the remaining were from urban areas 80 (38.1%). Considering social habits, 81 (38.5%) were found to be present with at least one social habit. Out of this, 23 (10.9%) were found to have the habit of smoking, whereas 25 (11.9%) were found to be alcoholic, and the remaining 33 (15.7%) were having mixed patterns of social habits (Table 1).
| Sl. No. | Categories | Sub-categories | No of participants N=210 |
|---|---|---|---|
| 1. | Gender | Male Female | 76.6% (161) 23.3% (49) |
| 2. | Age | 60-69 70-79 80-89 90-99 | 55.2% (116) 33.8% (71) 8.09% (17) 2.8% (6) |
| 3. | Residence | Rural Urban | 61.9% (130) 38.1% (80) |
| 4. | Social habits | Smoking Alcoholic Mixed | 10.9% (23) 11.9% (25) 15.7% (33) |
| 5. | Literacy | Literate Illiterate | 34.3% (72) 65.7% (138) |
Demographics Details of the study participants.
Distribution of Comorbidities in the study population
Among overall population, 193 (91.9%) subjects were reported with comorbidities. The most common chronic diseases were hypertension (43.4%), followed by type 2 diabetes mellitus (21.3%) and the least was found to be Hypothyroidism (1.6%) (Table 2).
| Sl. No. | Co-Morbidities | Frequency (n) | Percentage (%) |
|---|---|---|---|
| 1. | Hypertension | 134 | 43.4 |
| 2. | Type 2 Diabetes | 66 | 21.3 |
| 3. | IHD | 45 | 14.8 |
| 4. | Chronic liver disease | 15 | 4.8 |
| 5. | Chronic kidney disease | 13 | 4.2 |
| 6. | COPD | 12 | 3.9 |
| 7. | TB | 8 | 2.5 |
| 8. | Rheumatoid arthritis | 6 | 1.9 |
| 9. | Asthma | 5 | 1.6 |
| 10. | Hypothyroidism | 5 | 1.6 |
| 11. | Total | 309 | 100 |
Distribution of co-Morbidities.
The average number of comorbidities per patient is 2.3 respectively. Comorbidities were assessed based on Charlson Comorbidity Index (CCI), where mean score of comorbidities is 3.86 with 54% survival rate in 10 years.
Distribution of DRPs based on PCNE classification
Out of 210 patients, 132 subjects presented with 299 DRPs. Majority were found in males 104 (78.8%) followed by female 28 (21.2%), Out of 210 prescriptions, 80 (38.09%) prescriptions were found to have 107 DDIs. All the drug-drug interactions were assessed using IBM Micromedex software. The identified DDIs were categorised as major, moderate, and minor based on severity. Among 107 DDIs identified, 61 (57%) were found to be major, 40 (37.38%) were found to be moderate and 6 (5.6%) were found to be minor (Figure 1).

Figure 1:
Total number of Drug-Drug Interactions in the study population.
The most frequently identified interacting pair of drugs was aspirin+furosemide 18 (16.8%), followed by aspirin+clopidogrel 12 (11.21%), metronidazole+ondansetron 9 (8.41%) with major severity. Followed by aspirin+metoprolol 4 (3.73%) with moderate severity and furosemide+theophylline 2 (1.8%) with minor severity. Out of 299 DRPs identified, aspirin 46 (15.38%) was the drug associated with majority of DRPs, followed by furosemide 25 (8.36%), ondansetron 21 (7.02%) and metronidazole 18 (6.02%). Other DRPs are found within the Problem domain (23.07%), Cause domain (43.47%), planned interventions (16.72%), Intervention acceptance (11.70%) followed by Outcome domain (5.01%) of PCNE classification (Table 3) (Figure 2).
| Code | Primary domains | Frequency of problems | |
|---|---|---|---|
| Problems | P | 69 (23.07%) | |
| P1 | Treatment effectiveness | 48 (16.05%) | |
| P2 | Treatment safety | 1 (0.33%) | |
| P3 | Other | 20 (6.6%) | |
| Cause | C | 130 (43.47%) | |
| C1 | Drug selection | 22 (7.35%) | |
| C2 | Drug form | 2 (0.66%) | |
| C3 | Dose selection | 6 (2%) | |
| C4 | Treatment duration | 6 (2%) | |
| C5 | Dispensing | 5 (1.6%) | |
| C6 | Drug use process | 9 (3.01%) | |
| C7 | Patient related | 35 (11.70%) | |
| C8 | Patient transfer related | 4 (1.3%) | |
| C9 | Other | 41(13.7%) | |
| Planned interventions | I | 50 (16.72%) | |
| I1 | At prescription level | 7 (2.3%) | |
| I2 | At patient level | 24 (8.02%) | |
| I3 | At drug level | 18 (6.02%) | |
| I4 | Other | 1 (0.33%) | |
| Intervention Acceptance | A | 35 (11.70%) | |
| A1 | Interventions accepted | 23 (7.69%) | |
| A2 | Intervention not accepted | 7 (2.3%) | |
| A3 | Other | 5 (1.6%) | |
| Status of DRPs | O | 15 (5.01%) | |
| O0 | Problem status unknown | 2 (0.66%) | |
| O1 | Problem solved | 10 (3.3%) | |
| O2 | Problem partially solved | 3 (1%) | |
| Total number of DRPs | 299 |
Distribution of DRPs as per PCNE classification V.9.1.
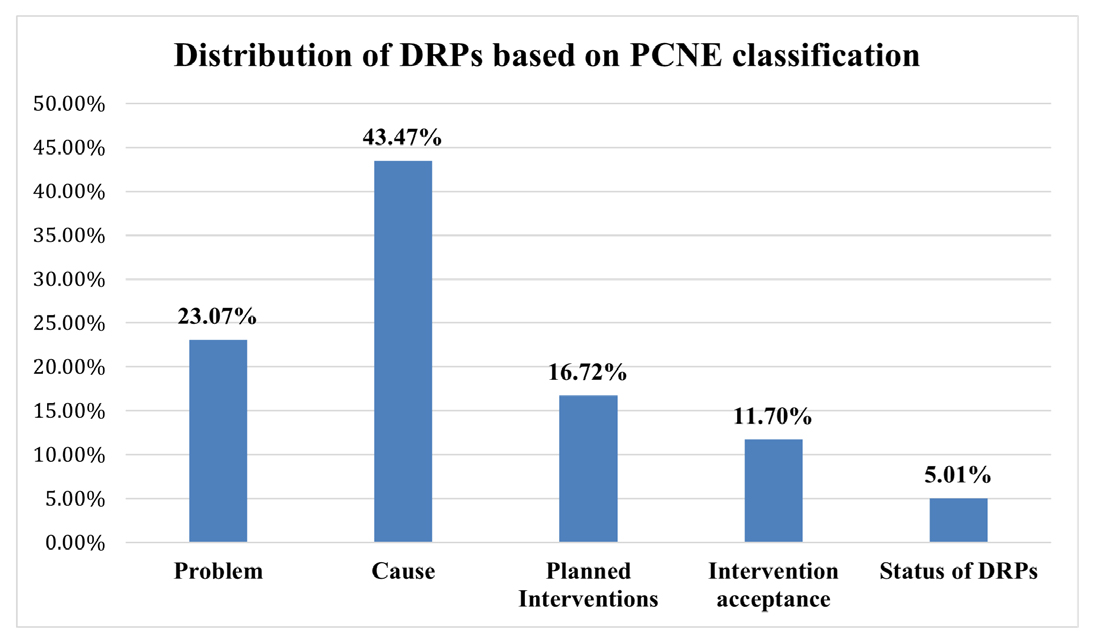
Figure 2:
Distribution of DRPs based on PCNE classification.
Overall, 299 DRPs were found from 132 (62.8%) study population. 69 (23.07%) of DRPs were observed in (treatment effectiveness, treatment safety, unnecessary drug treatment and unclear problem/complaint) problem domain of PCNE classification. The most commonly found DRPs in problem domain were treatment effectiveness related which involves the effect of drug treatment not optimal 24 (8.02%), followed by untreated symptoms or indication 18 (6.02%), unnecessary drug treatment 14 (4.68%).
Among 299 DRPs identified 130 (43.47%) were observed in cause domain, in which 7.3% belong to drug selection, out of which the majority of causes are no or incomplete drug treatment in spite of existing indication 21(7.02%). Followed by inappropriate drug according to guidelines/formulary 16 (5.35%), no indication for drug 2 (0.6%).
The second least DRPs were found in planned interventions 50 (16.72%), which were found to be at various levels such as at prescriber level, patient level, drug level, and other interventions. The least DRPs were found in Intervention acceptance 35 (11.70%) and intervention outcome 15 (5.01%) domains of PCNE classification.
DISCUSSION
The study includes a total of 210 subjects based on inclusion and exclusion criteria. Among 210 Subjects, 161 (76.6%) were males and 49 (23.3%) were females. Majority of subjects belong to the age group of 60-69 years 116 (55.24%) and the least exist in >90 years of age group 6 (2.85%). Research conducted by Hailu et al., showed similar results, males (54) were predominant, and majority of subjects were found in age group of 60-70 years and (68.5%) majority of participants reside in rural areas.1 Among overall study population, 193 (91.9%) were reported with 309 comorbidities, and hypertension was most dominant (43.3%) comorbidity followed by type 2 DM (21.3%). Most of the subjects had CCI score 3 or greater with 54% survival index and 207 (98.5%) prescriptions had polypharmacy. A study conducted by Mathumalar Loganathan Fahrni et al., which showed majority of diseases belongs to cardiovascular system and CCI score of 3 with 52% mortality rate and 301 patients had polypharmacy.10
Out of 210 subjects, 132 (62.8%) subjects were identified with 299 DRPs. In this study, the incidence of DRPs was more significant in males 104 (78.7%) than in females 28 (21.2%). This may have been seen because males have higher tendency to smoke and consume alcohol due to their workload and family pressure, which worsens their health condition and results in complications leading to polypharmacy which causes an increase in the DRP occurrence and also a greater number of patient cases collected for our study was males. A similar study conducted by Megha Sunny et al., reported male 210 (60.0%) predominance over female 114 (40.0%) and shows a higher incidence of DRPs in males 150 (58.8%) over females 104 (41.2%).15
The most commonly reported DRPs were drug-drug interactions 107 (35.78%) followed by indications without drug 17 (5.68%), and drug-food interactions 18 (6.02%). A study conducted by Samuel Berihum Dagnew et al., that the most frequently encountered DRP was drug-drug interactions.16 DRPs are associated with treatment effectiveness where the effect of drug treatment is not optimal 24 (8.02%), followed by untreated symptoms/indications 18 (6.02%), unnecessary drug treatment 14 (4.68%). This coincides with the research conducted by Berhane Yohannes Hailu et al., where the incidence of DRPs is associated with treatment effectiveness and treatment safety.1
We observed that the subjects with Cardiovascular Diseases (CVD) are more prone to DRPs followed by DM, and respiratory tract infections. This may be because cardiovascular diseases need long-term treatments and are frequently associated with co-morbidities and complications which ultimately lead to multiple drug administration and thus predispose to drug-related problems. Similar research committed by Ding-cheng Chan et al., found that patients with cardiovascular diseases are at higher risk of developing DRPs.17
To identify the associated factors, the result of our study reports that polypharmacy, illiteracy and patients with low socio-economic status with the important risk factors associated with the DRPs. This is because most of the subjects had one or more comorbidities which necessitate prescribing an additional number of drugs. Research conducted by C. Shinu et al., also showed a similar association between polypharmacy, illiteracy and low economic status for causing DRPs.12
CONCLUSION
The research suggests that avoiding inappropriate drug use can help patients, doctors and other healthcare professionals to reduce the drug-related problems and other complications of drug therapy. The drug-related problems like drug-drug interaction followed by ADR, Indication without drug and therapeutic duplication are more frequent in hospitalized patients. Most of DRPs identified were of major severity. The study findings showed that the most prevalent drug class and drug involved in DRP was cardiovascular drugs like aspirin. Clinical pharmacists can effectively identify, minimize, resolve and report the different types of DRPs occurring in subjects. DRPs can be avoided through rational drug use, proper patient education and cautious monitoring. Therefore, the regular involvement of clinical pharmacists in ward rounds accelerate the process of reorganization of DRPs and may reduce the occurrence of DRPs, and hospital visit, thereby improving the patient’s overall health-related quality of life.
Cite this article
Nyamagoud SB, Swamy AHV, Purantar AM, Jangliwale BK, Kumar K, Rakshitha TP. Assessment of Drug-Related Problems in Geriatric Patients of Tertiary Care Hospital: A Prospective Observational Study. Int. J. Pharm. Investigation. 2024;14(2):386-91.
ACKNOWLEDGEMENT
The authors are thankful to the Vice-Chancellor, Registrar and Dean of Pharmacy, KLE Academy of Higher Education and Research, Belagavi. We would also like to thank Medical and Hospital Staff of Vivekanand General Hospital, Hubballi for providing necessary support.
ABBREVIATIONS
| DRP | Drug related problems |
|---|---|
| ADR | Adverse drug reactions |
| DDI | Drug-drug interaction |
| CCI | Charlson comorbidity index |
References
- Hailu BY, Berhe DF, Gudina EK, Gidey K, Getachew M. Drug related problems in admitted geriatric patients: the impact of clinical pharmacist interventions. BMC Geriatr. 2020;20(1):13 [PubMed] | [CrossRef] | [Google Scholar]

- Baré M, Lleal M, Ortonobes S, Gorgas MQ, Sevilla-Sánchez D, Carballo N, et al. Factors associated to potentially inappropriate prescribing in older patients according to STOPP/START criteria: MoPIM multicentre cohort study. BMC Geriatr. 2022;22(1):44 [PubMed] | [CrossRef] | [Google Scholar]

- Ramanath KV, Nedumballi S. Assessment of medication-related problems in geriatric patients of a rural tertiary Care Hospital. J Young Pharm. 2012;4(4):273-8. [PubMed] | [CrossRef] | [Google Scholar]

- Dong PTX, Pham VTT, Dinh CT, Le AV, Tran HTH, Nguyen HTL, et al. Implementation and evaluation of clinical pharmacy services on improving quality of prescribing in geriatric inpatients in Vietnam: an example in a low-resources setting. Clin Interv Aging. 2022;17:1127-38. [PubMed] | [CrossRef] | [Google Scholar]

- ElDesoky ES. Pharmacokinetic-pharmacodynamic crisis in the elderly. Am J Ther. 2007;14(5):488-98. [PubMed] | [CrossRef] | [Google Scholar]

- Jayakumar A, Abraham AS, Kumar S, Chand S, George SM, Joel JJ, et al. Critical analysis of drug-related problems among inpatients in the psychiatry department of a tertiary care teaching hospital: a pharmacist led initiative. Clin Epidemiol Glob Health. 2021;11:100743 [CrossRef] | [Google Scholar]

- Elderly NSO. 2021 Available fromhttps://mo spi.gov.in/web/mospi/reports-publications
India. In: New Delhi: National Statistical Office, Ministry of Statistics and Programme Implementation, Government of India.
- Modig S, Holmdahl L, Bondesson Å. Medication reviews in primary care in Sweden: importance of clinical pharmacists’ recommendations on drug-related problems. Int J Clin Pharm. 2016;38(1):41-5. [PubMed] | [CrossRef] | [Google Scholar]

- van den Bemt PM, Egberts TC, de Jong-van den Berg LT, Brouwers JR. Drug-related problems in hospitalised patients. Drug Saf. 2000;22(4):321-33. [PubMed] | [CrossRef] | [Google Scholar]

- Fahrni ML, Azmy MT, Usir E, Aziz NA, Hassan Y. Inappropriate prescribing defined by STOPP and START criteria and its association with adverse drug events among hospitalized older patients: A multicentre, prospective study. PLOS ONE. 2019;14(7):e0219898 [PubMed] | [CrossRef] | [Google Scholar]

- Shetty V, Chowta MN, Chowta K N, Shenoy A, Kamath A, Kamath P, et al. Evaluation of potential drug-drug interactions with medications prescribed to geriatric patients in a tertiary Care Hospital. J Aging Res. 2018;2018:5728957 [PubMed] | [CrossRef] | [Google Scholar]

- Roy DA, Shanfar I, Shenoy P, Chand S, Nandakumar UP, Bharthraj KC, et al. Drug-related problems among chronic kidney disease patients: a pharmacist led study. Int J Pharm Sci Res. 2020;12(04):79-84. [CrossRef] | [Google Scholar]

- Shinu C, Dilip C. Impact of pharmaceutical care programme on health outcome of geriatric patients. Clin Epidemiol Glob Health. 2020;8(3):894-8. [CrossRef] | [Google Scholar]

- Sanija P, Nandakuar UP, Shetty J, Bharathraj KC, Vinay BC, Chand S, et al. Adverse drug reactions and its management associated with cancer chemotherapy. Int J Pharm Pharm Sci. 2020;11(04):5828-35. [CrossRef] | [Google Scholar]

- Sunny MKN, Aathif M, Subramanya C, Chand S, Up N. Assessment of drug-related problems among geriatric inpatients: an APS-Doc Classification System-based study. Aging Healthc. 2022;13(4):163-9. [CrossRef] | [Google Scholar]

- Dagnew SB, Binega Mekonnen G, Gebeye Zeleke E, Agegnew Wondm S, Yimer Tadesse T. Clinical pharmacist intervention on drug-related problems among elderly patients admitted to medical wards of Northwest Ethiopia Comprehensive Specialized Hospitals: A multicentre prospective, observational study. BioMed Res Int. 2022:8742998 [PubMed] | [CrossRef] | [Google Scholar]

- Chan DC, Chen JH, Kuo HK, We CJ, Lu IS, Chiu LS, et al. Drug-related problems (drps) identified from Geriatric Medication Safety Review Clinics. Arch Gerontol Geriatr. 2012;54(1):168-74. [PubMed] | [CrossRef] | [Google Scholar]


