ABSTRACT
Due to the imbalanced patient-to-healthcare professional ratios, the increased workload for those who provide care, different adverse reactions of modern medicine, the inability to completely cure long-term ailments, expensive new medications and the emergence of novel disorders, all together have recently led to alternative medicine to attract renewed public interest. Utilizing complementary and alternative therapies can be beneficial for certain individuals. Alternative and complementary therapies are not included in standard medical care. Alternative, complementary, or integrative are terms utilized to explain medical procedures which are not considered to be a division of conventional Western medical practice. Alternative therapy comprises a wide range of disciplines, covering everything from your nutrition and exercise routine to your lifestyle and mental preparation. Herbal medicines, yoga, aromatherapy, dietary supplements, exercise, etc., are an example of alternative therapeutics.
INTRODUCTION
In the United States, Cardiovascular Disease (CVD) is the main factor in both male and female fatalities. In the US, heart disease takes the lives of 695,000 individuals annually, or one out of every five fatalities (Tsaoet al., 2023). Coronary Heart Disease, the most prevalent kind of CVD, claims the lives of over 358,000 individuals annually and charges the US $108,900 million. CVD health risks comprise high blood pressure, diabetes high LDL cholesterol, being obese, eating poorly, being inactive and drinking alcohol excessively (HDF, 2023). Based on standardized conventional therapy, an increasing number of practitioners have successfully used Complementary and Alternative Medicine (CAM) in the prevention and treatment of CVDs in recent years (Chenet al., 2012).
Changes in emotion, thinking and behavior are symptoms of mental diseases. Discomfort and/or complications managing Daily activities at work, at home, or in social circumstances can be signs of mental illness. Many persons who suffer from mental illnesses are reluctant to discuss them. However, mental illness is not a cause of shame. Like heart disease or diabetes, it is a medical issue. Additionally, mental health issues are treatable. As our knowledge of human brain functioning continues to grow, people can successfully manage their mental health disorders with the use of medications and other therapies (Mental Illness, 2024). Around 970 million individual’s worldwide battle with some form of mental illness or drug addiction. 1 person in every 4 persons is affected by mental illness at some point in their life. Mental diseases are responsible for 8 million deaths annually or 14.3% of fatalities worldwide (MHT, 2024).
Mental illnesses range from cognitive impairment and autism in children to anxiety, substance misuse and depression in maturity. Even geriatric people also suffer from mental illnesses such as dementia. Besides the above-mentioned diseases, there are many mental health problems including stress, trauma, anger, loneliness, eating problems, bipolar disorder, hearing voices, phobias, schizophrenia, self-harm, body dysmorphic disorder, obsessive-compulsive disorder, post-traumatic stress disorder, mania, panic attacks, sleep problems, psychosis, anger etc., (Org.uk, 2024).
CAM has gained international attention over the past ten years. According to current estimates, a significant section of the inhabitants in many evolving nations anticipates significantly on healers of traditional and medicinal herbs to address basic healthcare needs. Although some nations may have access to modern medicine, herbal medicines have frequently maintained their appeal due to historical and cultural factors. In parallel a lot of people in wealthy nations have started using CAM including herbal remedies. The WHO predicted that by 2050, the global market of herbal medicines and herbal products would be worth 5 trillion US dollars (Ajazuddinet al., 2012). CAM is a wide-ranging category of healing practices that includes all modes, practices and theories related to health that are not fundamental to the government’s authority and are related to the system of health in a present culture or society at a particular time in history. CAM comprises any methods and theories that are deemed by its practitioners to be effective in preventing or treating disease or enhancing health and well-being. There aren’t usually clear or defined boundaries inside CAM or between CAM’s domain and the dominant systems (Ernstet al., 2000).
CLASSIFICATION OF CAM
The classification of CAM therapies is given in Figure 1.
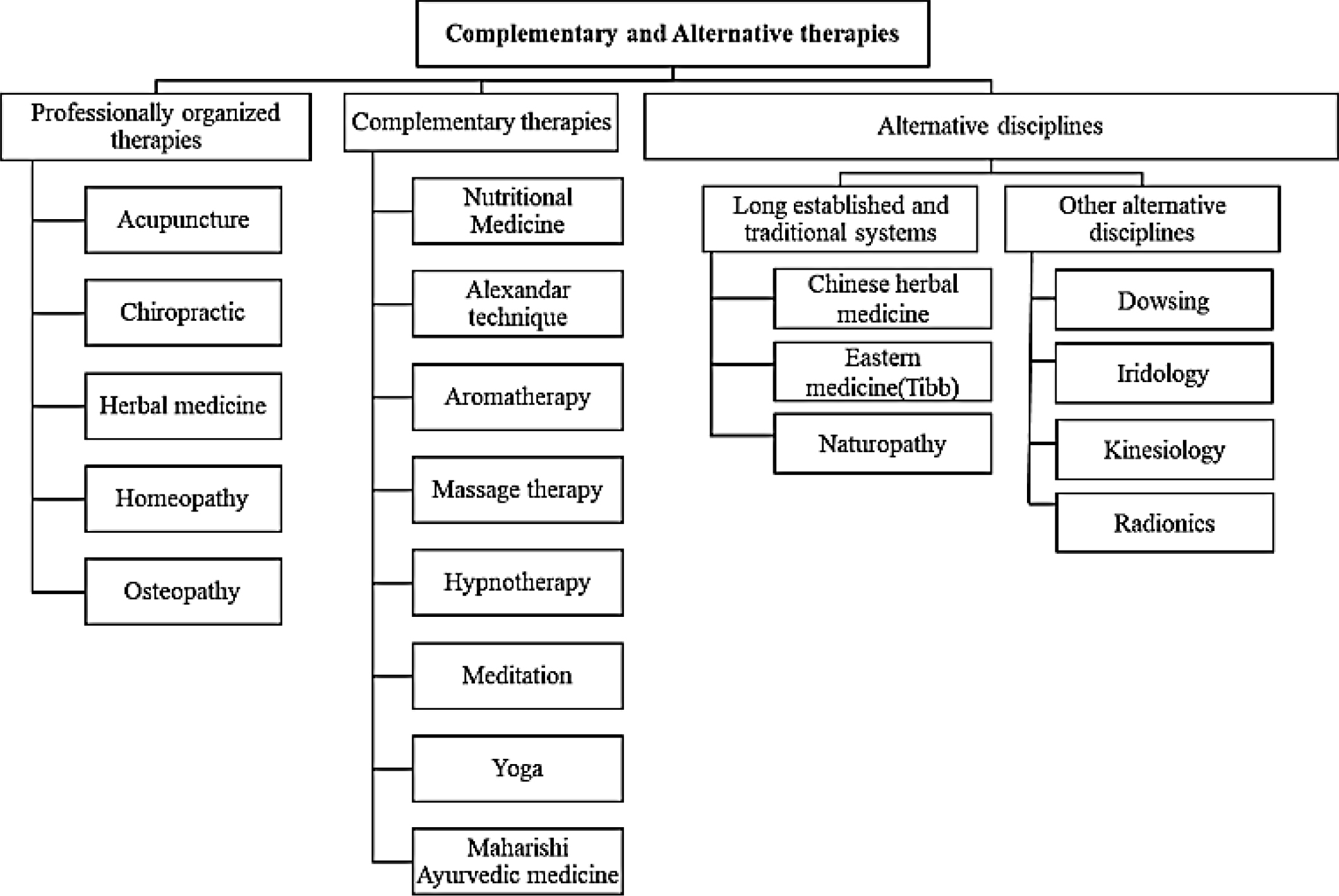
Figure 1:
Classification of CAM therapies.
“The National Center for Complementary and Alternative Medicine (NCCAM)” categorizes CAM treatments into,
- Energy medicine.
- Biological-substance-based treatment.
- Traditional medical techniques like whole medical systems.
- Manipulative and body-based treatment.
- Mind-body therapy (NCCIH, 2024).
Energy medicine
Energy medicine is a sub-specialty to interrelating medicine which focuses on study relating to the curative uses of precise energies. Western or Allopathic medicine has studied the body’s internal processes for centuries, starting with tissues, cells and organs which progress on the present-day notion of hormones and peptides. Contemporary medicines place a lot of emphasis on physiology, yet the human body includes many non-physical components that produce and take in an enormous amount of information. By interacting with its surroundings through ambient fields like light, sound, electricity and magnetism as well as with all other living organisms, physiology produces energy fields with enormous volumes of details.
Biological-substance based treatment
This kind of CAM makes use of natural resources. Examples include vitamins, which the body needs in small doses to function and maintain health; dietary supplements, which are products that are added to the diet and may contain substances like vitamins, minerals and herbs; and botanicals, which are actual plants or portions of plants. Cannabis is one kind and specific meals or diets; and herbs and spices like turmeric or cinnamon.
Manipulative and body-based treatment
These are based on manipulating one or more bodily parts. Examples include massage therapy, which involves massaging, tapping, kneading and stroking the body’s soft tissues; chiropractic therapy, which involves manipulating the spine, joints and skeletal system; and reflexology, which involves applying pressure to specific pressure points on the feet or hands that are thought to correspond with various body parts.
Traditional medical techniques like whole medical systems
These belief systems and methods of healing have developed over time in various societies and civilizations. Several instances are:
Ayurvedic medicine: an Indian system whose objective is to purify the body and bring back harmony to the body, mind and soul. It makes use of dietary restrictions, natural remedies, physical activity, breathing exercises and other techniques.
Traditional Chinese medicine is predicated on the idea that qi, or the body’s life force, travels along meridian channels and maintains equilibrium in a person’s physical, mental, emotional and spiritual well-being. It seeks to reestablish the harmony between the yin and yang energies in the body.
In Chinese medicine, acupuncture is a widespread procedure that includes stimulating certain body spots to enhance health, reduce disease symptoms and/or mitigate the negative effects of medication.
Naturopathic medicine is a non-drug and non-surgical medical system. It is predicated on the utilization of all-natural healing aids like air, water, light, heat and massage. Acupuncture, diet, herbal items and aromatherapy are further potential uses.
Mind-body therapy
Mind-body therapies seek to increase the mind’s beneficial impact on the body. Spiritual, mental, community, creative and behavioral procedures make use of a variety of methods.
Although the concept of the mind-body link is not new, some people in the West who have been raised believing that the body and the mind are two separate things can find it strange. However, as scientists continue to demonstrate the intricate connections between the mind and body, this viewpoint is quickly transforming.
Mind-body treatments include
- Meditation Prayer.
- Behavioral and cognitive treatment.
- Directed imagery.
- Biofeedback.
- Yoga (MBT, 2024).
CAM THERAPIES FOR ANXIETY DISORDER, INSOMNIA, AUTISM SPECTRUM DISORDER (ASD), DEMENTIA
The most prevalent psychiatric disorder is anxiety, with a lifetime prevalence of 29% in the general population. Particularly in older people, the high frequency and complex comorbidity of sleeping or anxiety issues like sleeplessness raises concerns because they hurt physical and mental health and lower quality of life due to their link to significant clinical implications in conditions like cardiovascular disease, obesity, neurological disorders and hypertension. It is well known that treating anxiety or insomnia may have beneficial consequences, not only by reducing multimorbidity but also by averting future occurrences. Alternative therapies, such as herbs, vitamins, rest and exercise, meditation and acupuncture, can be used to treat insomniacs. The most widely utilized therapies are those that are biologically based, such as mind-body therapy and nutritional or herbal medicine. For instance, herbal pills, especially those containing Valerian root and chamomile, may help people sleep better and fall asleep more quickly, however, additional research is required to determine their safety. The major hormone responsible for the sleep-wake cycle, melatonin is made by the pineal gland and controls a wide range of biological processes, comprising sleep, immunity, circadian rhythm, ageing and stress response.
Nonrandomized clinical investigations on older persons have shown that using lavender (Lavandula angustifolia) in aromatherapy raises serum melatonin levels. Additionally, moderate exercise, relaxation techniques like yoga and meditation and acupuncture may all help with sleep issues like insomnia. Recently, COVID-19-positive patients have been seen to experience the highest extent of anxiety, distress, despair, panic, emotional outbursts and sleep difficulties, especially as a result of quarantine events and isolation. Few sedatives and anti-anxiety medications are employed to control the previously mentioned symptoms, but they may impair breathing and make the illness worse. Beyond the negative consequences, evidence suggests that COVID-19 patients can use the progressive muscle relaxation approach to lower anxiety and enhance sleep quality.
Music has a strong emotional impact on us and therapies like mind-body medicine directly affect our ability to combat anxiety. The emotional, physiological and cognitive effects of stress may be immediately improved by listening to music. It increases physiological coherence, lowers the cortisol ratio and strengthens immunity while enhancing parasympathetic activity. According to a comprehensive evaluation of 23 surveys on physiological characteristics, music therapy has a proven ability to reduce anxiety in each study. Additionally, studies have shown that music might alleviate sleep disorders by boosting comfort and lowering anxiety. As a result, strong anti-anxiety drugs may be partially replaced by robust procedures, increasing the quality of life for these individuals.
“Autism Spectrum Disorder (ASD)” is a diverse class of neurologic developmental diseases that are specified by a limited, monotonous and stereotyped sequence of behavior and interests as well as poor social interactions and communication. Although there is currently no definitive pathogenesis for ASD, it is believed that genetic and environmental variables play a significant role in its etiology. Even though autism spectrum disorder is a lifetime condition for which there is now Alternative Medicine (AM) and no known cause therapy, AM may offer a therapeutic approach to treating its symptoms.
ASD can be treated with biologically based therapies such as vitamin and mineral supplements and herbal medicines like Queen of the Meadow, marshmallow root, calendula, lemon balm and chamomile. ASD can also benefit from the use of energy medicine, such as reiki or homoeopathy and body-based practices, namely acupuncture, chiropractic treatment, massage and, as well as mind-body medicine, such as yoga, art, music, dance and prayer. Children with autism may benefit significantly from music therapy. A Cochrane meta-analysis revealed that music listening considerably increased autistic children’s capacity for collaboration and communication.
According to another study, music therapy may offer a foundational and supporting kind of treatment for kids with retarded speech development. The scientific community has taken note of various research that highlighted the value of selected alternative therapies (such as equine therapy), but there is not enough data to decide the safety and effectiveness of AM. Therefore, patients with functional disorders like autism may benefit from a combination of conventional medical therapies and secure alternative methods including nutrition, exercise and lifestyle modification (Akteret al., 2021). Aromatherapy is one type of CAM that involves applying essential oils topically, or less frequently, orally, as a form of treatment. Nowadays, aromatherapy is a distinguished method of treatment by the WHO. It is frequently used to treat anxiety and everyday stress issues as well as to reduce pain, elevate mood and induce relaxation (Exploring aromatherapy, 2024).
For dementia, laughter holds a special place in CAM. Long recognized as having positive effects on human health, laughter has been linked to enhanced endocrinological and immunological responses as well as increased pain tolerance (Takedaet al., 2010; Stuberet al., 2009). As group programs and self-management strategies, laughter therapy, humor sessions, laughter meditation and laughing groups each have specific implications.
Why CAM for Mental health issues?
Psychiatric drugs can occasionally be a contentious subject. Mental health drugs are thought to be necessary for treating mental diseases, but others believe they are prescribed in more instances than obligatory and may have unintended side effects. The type of mental health medication that is most frequently administered is an antidepressant (such as an SSRI, or selective serotonin reuptake inhibitor). Common uses for them include the treatment of eating disorders, anxiety disorders and major depressive disorder. The brain’s serotonin levels are raised by antidepressants. Uncommon but possibly dangerous adverse effects of SSRIs and SNRIs include serotonin syndrome. Rarely, some persons who start taking antidepressants may have hopeless thoughts and a desire to hurt themselves. People under 25 appear to be in greater danger.
Drugs prescribed for mental health illness
- The primary classes of pharmaceuticals used to treat schizophrenia in patients are antipsychotics. Additionally, they are utilized in those who have psychosis, which might be a symptom of bipolar disorder, depression, or Alzheimer’s disease. First and second-generation antipsychotics are the two primary categories of antipsychotics. Psychosis is often treated with first-generation antipsychotics. Major depressive disorder, bipolar disorder and schizophrenia are the three disorders that are generally treated with second-generation antipsychotics.
- Bipolar disorder and personality disorders are often treated with mood stabilizers. By balancing out the extremes brought on by bipolar disease, mood stabilizers help.
- For the management of “Attention Deficit Hyperactivity Disorder (ADHD)”, stimulants are frequently employed. Stimulants function by raising dopamine levels in the brain.
- The medical word for anti-anxiety drugs is anxiolytics. Anxiolytics are a category of psychoactive drugs which are prescribed to manage anxiety disorders. Typically, anxiety-reducing medications encourage relaxation and anxiety reduction.
The Drawbacks of Mental Health Drugs
Although taking medication can change your life, not everyone can benefit from it. Treatment for psychiatric problems like ADHD, depression, anxiety and others frequently involves experimenting with various dosages and medication combinations to find the one that will work best for you. As a result, determining the drug and dosage that will perform the best for you can take a lot of time. Additionally, some individuals may develop negative side effects from taking drugs for mental health, such as weight gain, lightheadedness, or weariness. A few of the possible drawbacks are as follows;
- Not everyone responds well to psychiatric drugs and their effects can take even weeks or months to be noticeable.
- Some persons who use psychiatric drugs report adverse effects like weight gain, exhaustion, erectile problems, or vertigo (Pros and cons of mental health medications, 2023).
The allopathic and alternative medicines available for some mental health issues are given in Table 1 and Figure 2a represent the percentage of people using CAM therapies for mental health illness in the United States.

Figure 2:
A: Percentage of people using CAM therapies in the United States. B: Percentage of people using CAM therapies for CVDs.
| Sl. No. | Mental health Issue | Medicine availability in allopathy | Alternative Medicine |
|---|---|---|---|
| 1. | Anxiety | Clonazepam, Alprazolam | Mindfulness meditation |
| 2. | Autism | Risperidone, Aripiprazole | Speech therapy |
| 3. | Insomnia | Zolpidem, Triazolam | Chammomile |
| 4. | Dementia | Donepezil, fluoxetine | Coral calcium, acupuncture |
| 5. | Panic attacks | Sertraline, Paroxetine | Kava kava, St. John’s wort |
| 6. | Depression | Citalopram, Escitalopram | Acupuncture |
| 7. | Bipolar Disorder | Carbamazepine, Valproic acid | Calming techniques like yoga, massage therapy, acupuncture, meditation |
Medicines available in allopathy and alternative medicine for mental health issues.
CAM THERAPIES FOR CARDIOVASCULAR DISORDERS (CVDS)
More people are exploring choices in their medical care, including alternative medicines, to cure and prevent future progression of their condition as the incidence of heart disease rises along with our ageing population. The Complementary and alternative treatments may provide options for patients who are having Heart Failure (HF) beyond the conventional HF treatment regimen Iridology, Aromatherapy, diet-based therapies, traditional medicine, chelation treatment, phototherapy/herbal medicine, megavitamin treatment and neural treatment, are examples of physiologically based remedies (Clinic, 2024; Chowet al., 2023). Numerous therapies are holistic, to treat the patient as a whole while promoting their overall health. This method involves treatments that may affect one’s body, mind, emotions, or soul. These could range widely, from acupuncture to guided visualization, nutritional advice to herbal remedies (Grantet al., 2012). In addition to being an antioxidant scavenger, vitamin C also works in concert with vitamin E to weaken the peroxyl radical. Vitamin C prevents lipid peroxidation by capturing the peroxyl radicals in the water phase and also supports the normalization of endothelial vasodilatory function in heart failure patients by enhancing nitric oxide availability (Frishman, 2009).
Omega-3 polyunsaturated fatty acids (fish oil) derived from marine sources are frequently promoted as having significant cardiovascular protective effects via the hypothesized mechanisms of lowering triglyceride levels (for which they have FDA approval), preventing arrhythmias, lowering platelet aggregation, or lowering blood pressure (Rizoset al., 2012). The most popular way to utilize garlic is as a dietary supplement to treat hyperlipidemia, cardiovascular conditions and high blood pressure. A well-conducted, randomized experiment found no significant reduction in LDL-cholesterol, HDL-cholesterol, triglycerides, or the total cholesterol-HDL ratio after six months of therapy with three garlic preparations versus placebo. Garlic reduces blood pressure in patients having elevated systolic blood pressure (10-12 mM Hg, 6-9 mM Hg diastolic), but not among individuals with normal blood pressure (Onget al., 2008).
According to various studies, the antioxidant, antiplatelet, vasodilatory, antihypertensive and antithrombotic properties of ginkgo biloba have cardioprotective benefits (Brinkleyet al., 2010). A dietary regimen should be considered a foundation of prophylactic care and, perhaps of course, a therapeutic option for Blood Pressure (BP), Cardiovascular Disease (CVD) and other chronic disorders (Qidwaiet al., 2013). Some dietary supplements, like coenzyme Q10, multivitamins as well as fish oil, are regarded as the greatest preventative medicine (Darntonet al., 2011). Healthcare practitioners are increasingly using traditional medicine techniques like transcutaneous electric acupoint stimulation, acupuncture and electroacupuncture, despite the paucity of data supporting their effectiveness on CVDs (deet al., 2018).
Aesculus hippocastanum, Ginkgo biloba, Ginseng, Allium sativum and Salvia miltiorrhiza have all been utilized as medical herbs to treat patients with angina pectoris, congestive heart failure, hyperlipidemia, atherosclerosis and systolic hypertension (Rastogiet al., 2016). Many bioactive substances found in herbs can inhibit the phenotypic switching of vascular smooth muscle cells, endothelial dysfunction, activation of platelets, lipid peroxidation, formation of ROS and macrophage atherogenicity, which may be able to modulate the incidence of CVD (Shaitoet al., 2020). Zen Buddhist meditation, Mindfulness meditation, Mantra meditation and transcendental meditation, are only a few of the several types of meditation that are referred to as meditation. As an example, a meta-analysis discovered that transcendental or Vedic meditation decreased 4.7 mM Hg for systolic blood pressure and 3.2 mm Hg for diastolic blood pressure (Nahaset al., 2008). It has been claimed that osteopathic and chiropractic spinal manipulation are effective treatments for hypertension (Sullivanet al., 2020). Since alcohol (ethanol), which is present in red wine, appears to reduce insulin resistance and has antiplatelet effects, there may be benefits in lowering CV incidence from alcohol itself. Red wine polyphenols, in particular those that increase nitric oxide, may be beneficial for preventing cardiovascular disease in general (Wallerathet al., 2003).
Drawbacks of cardiovascular medications
Several heart and blood vessel problems are referred to as “Cardiovascular Diseases” (CVDs). They consist of congenital heart disease, coronary heart disease, deep vein thrombosis, cerebrovascular disease, rheumatic heart disease, hypertension, atherosclerosis, angina pectoris and myocardial infarction (Cardiovascular diseases, 2024). Different heart diseases are treated with an array of drugs. The following are some examples of medications used in cardiovascular medicine.
- Statins,
- Anti-coagulants,
- Vasodilators,
- Anti-platelet agents,
- Diuretics,
- Thrombolytic agents,
- Calcium channel blockers,
- ACE inhibitors, Angiotensin receptor blockers and,
- Beta blockers (Mandalet al., 2014).
In intensive care units, the endogenous catecholamines noradrenaline, adrenaline and dopamine are frequently administered to treat shock symptoms linked to acute cardiovascular diseases. Quick Intravenous (i.e.) bolus delivery of inadequately diluted adrenaline solutions can also cause cardiotoxicity (Goodman and Gilman’s, 2024). The nonselective-adrenoceptor agonist isoprenaline, sometimes referred to as isoproterenol, has a high risk of causing myocardial injury (Mladenkaet al., 2009). Cardioactive steroids have a low therapeutic index, which means that the therapeutic doses are extremely close to the toxic values. This is a significant drawback of their clinical use (Rathoreet al., 2003). The most frequent adverse reaction of ACE inhibitors is dry cough. Less frequently, these medicines lead to conditions like feeling dizzy, hunger reduction, restlessness, headache and high blood potassium levels, which can lead to issues with heart rhythm. Potential negative consequences of ARBs include clogged nose, leg and back discomfort, diarrhea and the presence of fluid under the skin causing swelling (Heart attack medicines, 2024).
Why CAM for CVDs?
In both observational research and clinical trials, the utilization of several CAM medications by patients with heart failure has been investigated. In some studies, the use of particular CAM medicines has been linked to improvements in outcomes for major adverse cardiac events, performance, overall quality of daily life and heart failure symptoms. CAM agents may be used to treat heart failure circumstances. CAM agents and their benefits in CVDs are given in Table 2 and the percentage of people using CAM therapies for CVD is represented in Figure 2b.
| CAM agents | Benefits in CVD |
|---|---|
| Omega-3-fatty acids | Decreased non-sustained ventricular tachycardia in idiopathic dilated cardiomyopathy. |
| Acupuncture | Eliminated surges in sympathetic activation during mental stress. |
| Yoga | Significance decreases in heart rate, blood pressure, improvements in strength and balance. |
| Tai chi | Reduction in systolic blood pressure. |
| Khella | It can inhibit vascular smooth muscle contraction and seems to dilate peripheral and coronary vessels and increase coronary circulation. The khellin constituent also acts as a vasodilator. |
| L-Arginine | Significant improvement in endothelium dependent vasodilation after 4 weeks. |
CAM agents and their benefits in CVD.
CAM FOR DIABETES
Hyperglycemia, improper protein and lipid metabolism, as well as particular lifelong difficulties impacting the kidneys, neurological system and the retina, are all features of the metabolic condition known as diabetes mellitus. Many health advocacy groups, including WHO, have identified diabetes mellitus as a global epidemic that is spreading (Diabetes, 2024). 5 kinds of oral medications have been licensed in the management of diabetes. Any patient for whom nutrition and physical activity are ineffective in achieving satisfactory control of blood sugar should get oral treatment. Despite a positive initial reaction, a sizable portion of patients may see a decline in the effectiveness of oral hypoglycemic medications. Meglitinide, sulfonylurea, thiazolidine, biguanide and alpha-glucosidase inhibitors are among the medications in this group. These medications can produce a variety of adverse effects, including weight gain from sulfonylurea due to hyperinsulinemia, weakness, fatigue, lactic acidosis from biguanides, diarrhea from alpha-glucosidase inhibitors and a rise in LDL cholesterol from thiazolidinediones (Halimet al., 2003).
Yoga is an ancient, traditional form of exercise that originated in India and combines psychological, physical and spiritual components. Its effectiveness in treating conditions involving asthma, hypertension, weight gain and psychiatric illness has been investigated for many years (Guptaet al., 2006). Yoga has also been investigated for managing type 2 diabetes complications as well as its symptoms (Malhotraet al., 2002). These research findings point to a statistically significant connection between yoga and diabetes. Additionally, those diabetic individuals who had pre-existing complications showed a considerable improvement from yoga practice (Inneset al., 2005). Even the prevention of diabetes can benefit from yoga practices. Yoga enhances well-being and increases love by regulating psychic and physical processes. There are various theories regarding the biochemical processes that connect yoga’s advantages to the control of diabetes (Sahayet al., 2007).
Massage therapy can be integrated into therapy for relaxation, but it also has extra advantages that diabetics may find particularly helpful. For nearly a century, massage has been advocated for diabetes patients (Elsonet al., 1998). The beneficial impact of massage on bringing blood glucose levels back to normal has been studied in three published studies based on two studies and one unreported preliminary investigation (MASSAGE Magazine, 2024). In China, treatment with acupuncture is a popular method of treating diabetes. In the United States, acupuncture is most well-known as a complementary treatment for chronic pain. However, throughout the past few decades, it has been utilized to treat diabetes and its complications. In addition to managing diabetes, acupuncture may be useful in avoiding and treating its complications (Chenet al., 1994). Momordica charantia has been traditionally used as a treatment for diabetes in folk medicine. Fresh juice and unripe fruit have been demonstrated to reduce sugar levels in blood in both human clinical studies and animal experimental models (Karunanayakeet al., 1990).
In the glucose sensitivity test, the use of 15 g of seed powder of Trigonella foenumgraceum being soaked with water dramatically reduced postprandial blood sugar levels in type 2 diabetes patients (Madaret al., 1988). Azadirachta indica also referred to as neem. It has been used for a very long time to treat diabetes. Aqueous neem leaf extract significantly decreases blood sugar levels and protects from adrenaline- and glucose-induced hyperglycemia (Satyanarayanaet al., 1978). The use of essential oils for therapeutic purposes, known as clinical aromatherapy, has a long history. Research has proven its effectiveness (Lawlesset al., 2014). The burden of managing a chronic, lifelong condition like diabetes can also be reduced by using essential oils. The broad concept of “stress management” can include biofeedback, meditation, cognitive behavioral therapy and imaging. Biofeedback is a therapy practice that uses a device to transmit information regarding psychological activity, such as the temperature of the skin or muscle tension, to impart how to regulate a maladaptive reaction to stress. In diabetic patients, three months of biofeedback and relaxation were linked to a considerable drop in total blood glucose compared to the control group (McGinniset al., 2005). Comparatively speaking to the general population, those having type 2 diabetes have a greater incidence of anxiety and mood disorders (Andersonet al., 2001).
According to chromotherapy, a lack of orange and yellow pigments in the body is typically the root of diabetes. There are two ways to treat sickness using color, by applying light filtered through various colored glasses and by using color-charged water either externally or internally. The color of the pancreas is lemon yellow. It is a diuretic and laxative. It stimulates the spleen, liver and brain. Diabetes can also be managed with the use of green and orange (Batkeet al., 2011). Micronutrients have been looked into as both preventative and therapeutic agents to treat diabetes types 1 and 2, as well as for typical complications of diabetes (Mooradianet al., 1994). One of the prevalent deficiencies of micronutrients in diabetes is magnesium insufficiency (de Valket al., 1999). Diabetes is more common in those with low amounts of vitamin E and some studies indicate that patients with diabetes have lower levels of antioxidants (Polidoriet al., 2000).
Drawbacks of conventional drugs for diabetes
Sulfonylureas cause weight gain, skin rash, low blood sugar and an unpleasant stomach. Biguanides/Metformin cause alcohol-related sickness, kidney problems, stomach issues, fatigue or dizziness and a metallic taste. Inhibitors of alpha-glucosidase lead to bloating, gas and diarrhea. Weight gain, liver disease risk, anemia risk and ankle or leg swelling are all side effects of thiazolidinediones. Meglitinides result in increased body weight and low blood sugar (Wattset al., 2019).
Why CAM for Diabetes?
No matter the kind of diabetes, patients must maintain blood glucose control with medication, as well as by following a diet and exercise regimen. The development of type 2 diabetes is a growing health issue in developing nations as a result of modernizing lifestyles. Patients having type 2 diabetes are typically put on a limited dietary regime and told to engage in physical activity, mostly for the motive of controlling their body weight. If diet, exercise and blood glucose control do not achieve the intended results, pharmaceutical therapy is recommended (Khoslaet al., 1995). Alternative therapies that can control diabetes more effectively and safely have been encouraged by the present oral anti-diabetic drug limitations regarding efficacy or safety, as well as the disease’s rise as a global epidemic.
REGULATIONS AND GUIDELINES FOR CAM IN DIFFERENT PARTS OF THE WORLD
Regulations for CAM in North America
Regulations for CAM in the US
CAM use has significantly increased within the US in the course of recent years. To investigate “unconventional medical practices,” Congress developed the Office of Unconventional Therapies in 1992. This office later changed its name to the “Office of Alternative Medicine (OAM)”. The National Centre for Complementary and Alternative Medicine (NCCAM) replaced OAM as its name in 1998. A division of the “National Institutes of Health” is NCCAM. In its book, Complementary and Alternative Medicine in the United States, The Institute of Medicine reported that more than a third of American adults utilize various types of Complementary and Alternative Medicine (CAM) and that annual visit to CAM providers exceed that of primary care physicians. “The Food and Drug Administration (FDA)” have noticed an increase in ambiguity regarding which law- “the Federal Food, Drug and Cosmetic Act (FD and C Act)” or the “Public Health Service Act (“the PHS Act”)”- is responsible for regulating specific products used in CAM.
CAM goods are not excluded from regulation under the FD and C Act or the PHS Act. This means that if an individual chooses to produce and sell natural juice from vegetables to be consumed during juice therapy for achieving optimal health, that product is subject to the Act’s and the FDA’s food regulations, including the HACCP system’s juice standards in 21 CFR part 120. Vegetable juice would additionally be regulated as a drug under the Act if taken as part of a disease treatment programmed instead of for general well-being.
An herbal medicine made to treat human arthritis. The herbal product would fall under the interpretation of a “drug” under “section 201 (g) (1) (B)” of the Act since it is to be utilized for the evaluation, treatment, mitigation and cure or prophylaxis of a particular disease (arthritis in humans), making it a “biologically based practice” in terms of CAM domains. Unless it is widely acknowledged that it is suitable to be utilized according to the circumstances established, proposed, or recommended on the labelling, among professionals competent by technological knowledge and expertise to assess the safety and efficacy of medications, the same herbal medicine would be a “new drug” as well according to module or section “201 (p) (1)” of the Act. The prerequisites of the act for premarket evaluation and “FDA” clearance are triggered by “new drug” status. Acupuncture is a Complementary and Alternative Medicine (CAM) practice that involves prodding, pulling heating up, using electrical current, or using herbal medications to stimulate energy lines (or “meridians”). This serves as an example of by what means a CAM product may be considered a “device” under the Act. Acupuncture needles, which are often used, are considered “devices” according to section 201 (h) of the Act since they are meant to be used for curing, mitigating, treating, or preventing disease in humans or altering the makeup or functioning of a human body. Although acupuncture itself is not regulated by us (see 21 CFR 880.5580), we do control acupuncture needles.
Some items utilized in CAM procedures may likely qualify as “cosmetics” under the Act. For instance, if a CAM practice involves massaging the body using a moisturizer, then moisturizer may qualify as a “cosmetic” if it is sprayed, poured, sprinkled or rubbed in the body to enhance or change the look. Yet, if the moisturizer’s purpose involves illness diagnosis, curing, reducing, managing, or mitigation, or if it affects the structure or function of the body, it may be controlled as a medicine. Deodorant products that additionally function as antiperspirants, moisturizers and makeup sold with protection from the sun claims and shampoos which additionally treat dandruff are some more instances of drug/cosmetic combos (Fda.gov. 2003).
Regulations for Aromatherapy in the United States
Both the practice of aromatherapy and the production of aromatherapy goods are currently unregistered and unregulated professions. The industry as a whole strives to follow existing safety and practice requirements and to keep abreast of any potential upcoming legislation about producing goods with an aromatherapy foundation. NAHA is committed to providing you with the most recent information on any proposed legislation. In terms of licensing, aromatherapy is not a legally recognized profession in the US. Many aromatherapy practitioners are also licensed in other fields, such as nursing, acupuncture, massage therapy, aesthetics, naturopathy, etc. It is extremely doubtful that we will see a license for aromatherapy any time soon because licensing is often profession-driven rather than government-driven (Ellwoodet al., 2003).
USFDA Regulations for dietary supplements
Dietary components and finished dietary supplement items are likewise regulated by the FDA. Dietary supplements are subject to different FDA regulations than “conventional” foods and medications. “The Dietary Supplement Health and Education Act of 1994 (DSHEA)” banned the promotion of contaminated or misbranded dietary supplements as well as dietary components by manufacturers and distributors. The “FD and C Act,” as amended by DSHEA and FDA regulations, stipulates whether these companies are responsible for reviewing the labelling and safety of their items before marketing to ensure that they meet all of those standards.
• The FDA has the authority to take legal steps once a product reaches the market if it is contaminated or improperly branded.
• Dietary supplements can contain two types of substances: “dietary components” and “other ingredients.” A dietary ingredient, as defined by the Federal Food, Drug and Cosmetic Act (FD and C Act), is any amino acid, mineral, botanical as well as any herb. It may also be a concentration, metabolite, component essence, or blend of any of the above-mentioned dietary constituents. Dietary supplements are often sold in formats including powders, capsules, gel caps, tablets, soft gels and liquids and contain substances like botanicals, vitamins, minerals, amino acids and enzymes. Other stuff, namely sweeteners, fillers, preservatives, binders, excipients and flavorings, may also be present in dietary supplements. On the Supplement Facts label, these “other ingredients” are stated separately from the dietary constituents (DSD, 2024).
Canada’s CAM Regulations
Alternative, Complementary and conventional drugs have been referred to as natural health supplements in Canada and they are governed by food and medicine laws. Natural health care goods comprise vitamin and mineral supplements, herbal medications and Ayurvedic, Native American and traditional Chinese treatments. There are numerous organizations for practitioners of CAM. The “Canadian Association for Chinese Medicine and Acupuncture (CMAAC)” was founded as a governmental organization in 1983. The CMAAC seeks to bring practitioners together and advocate before government agencies for the oversight of acupuncture and traditional Chinese medicine. With the backing of the World Health Organization, the World Federation of Acupuncture and Moxibustion Societies was established in 1987. The Canadian Complementary Medical Association was founded in 1996 by allopathic physicians in Canada who were interested in complementary and alternative medicine.
The Proposed regulatory structure for Natural Healthcare Products was written in March 2001. Requirements for natural products supplied in Canada are included in the Framework, including licensing of sites and products, acceptable manufacturing practices, labelling and packaging requirements, as well as reporting of adverse effects. Without overly restricting the market for natural health products, the goal is to address customer concerns about product safety and quality. The Therapeutic Products Programme of Health Canada recently established the “Expert Advisory Committee on Complementary Medicines” to convey scientific guidance on matters relating to the quality, safety and effectiveness of natural healthcare commodities (Who.int. 2024).
Regulations for CAM in Europe
Regulations for dietary or food supplements in the European Union
In the EU, food supplements are regulated as foods. Harmonized legislation governs the vitamins, minerals and compounds that can be used as sources in the creation of dietary supplements. To safeguard consumers from potential health concerns, the European Commission has recognized harmonized requirements for compounds other than minerals and vitamins and maintains a list of compounds whose use is banned since it is recognized or suspected that they may have detrimental effects on health (MBM, 2017).
International Guidelines for Herbal medication
“The International Regulatory Cooperation for Herbal Medicines (IRCH)”, founded in 2006, is a global network of regulatory organizations in charge of supervising herbal drugs. Its purpose is to strengthen herbal medicine regulation to protect and promote the safety and health of the public. Any national regulatory authority in charge of regulating herbal medicine regulation, in addition to national or sub-regional regulatory bodies, is eligible to join. Current members of IRCH (34 members)-as of September 2017.
There are 31-member countries and 3 members regional or sub-regional bodies depicted in Figure 3a and 3b.

Figure 3:
A: Member countries in International Regulatory Cooperation for Herbal Medicines (IRCH). B: Regional or Sub Regional bodies of International Regulatory Cooperation for Herbal Medicines (IRCH).
REGULATIONS FOR CAM IN ASIA-PACIFIC REGION
Regulations for CAM in China
Both the national healthcare system’s incorporation of conventional medicine and integrated education of health professionals is officially pushed in China (Zhanget al., 2000). “The Bureau of Traditional Medicine” emerged as a component of the “Central Health Administration” in 1984. The State Administration of Traditional Chinese Medicine was formed in 1986 (TM, 2000).
Regulations for CAM in Japan
Japanese societies involved with CAM are depicted in Figure 4.

Figure 4:
Japanese societies involved in CAM.
All Kampo medicines utilized throughout Japan are subject to the same rules as normal Western medical products. Kampo formulations given by physicians are among those covered by National Health Insurance. The “Central Pharmaceutical Affairs Council’s Subcommittee for the Kampo Medicines and Plant and Animal Products” has developed legislation governing Kampo medications as exclusive medicines. These laws additionally apply to prescription medications, accompanied by minor adjustments. In Japan, the Pharmaceutical Affairs Law makes no distinction between historic and allopathic medications; both varieties of preparations are governed by identical rules (Suzukiet al., 2004).
Regulations for CAM in Australia
Under the “National Registration and Accreditation Scheme (NRAS)” encouraged by the “Health Practitioner National Law Act, 2009” (together mentioned as the National Law as passed in every State and Territory), the Australian Health Practitioner Regulation Agency (AHPRA) got the single national oversight agency for health professional regulation in Australia on 1 July 2010.1 Ten national medical professional boards were established, with each jurisdiction requiring mirror legislation and each State and Territory requiring parallel legislation.
The original NRAS ten boards governed ten health professions that were already registered in all Australian states and territories: chiropractic, dentistry, medicine, nursing and midwifery, optometry, osteopathy, pharmacy, physiotherapy, podiatry and psychology. The amount of evidence required is determined by the product’s claims. The Committee defines traditional usage as documented or oral proof indicating an item has been employed for certain health-related or therapeutic purposes for three Western Pacific 147 generations or more. Homoeopathy is one of the exceptions to this rule. The regulations contain provisions for using medications as a single aspect of a complex treatment, treatments that mix several traditions and treatments that are current adaptations of traditional therapies (Sibbrittet al., 2018).
Regulations for CAM in India
The Government of India acknowledges Ayurveda, Unani, Siddha, Naturopathy, Homoeopathy and Yoga. “The Central Council of Indian Medicine Act of 1970 (2)” was the initial step towards obtaining this status. The Central Council’s main mandates are as follows: to standardize instruction by recommending a minimum level of education in traditional medicine, even though not every practitioner of traditional medicine and homoeopaths must be professionally trained to practice; to provide guidance to the central authority on circumstances associating with the identification/cancellation of medical credentials to conventional medicine in India; and to keep central registration of Indian medicine updated, to set norms of professional behavior and etiquette and to develop an ethical code for practitioners in traditional medicine within India. To practice, all practitioners of conventional medicine and homoeopaths must be registered.
The same mandates apply to the Central Council of Homoeopathy, which was established in 1973. The Department’s core areas of work are education, medicine standardization, raw material availability enhancement, development and research, information distribution, communication and the inclusion of conventional therapies and homoeopathy in national medical services. In these locations, almost 4000 people work. The Indian government wants to see traditional medicine and homoeopathy used actively and positively in public health initiatives, family benefit schemes and basic health protection (Gov.in. 2024).
REGULATIONS FOR CAM IN THE MIDDLE EAST AND AFRICA
Regulations for CAM in South Africa
“The Associated Health Service Professions Act of 1982”, as modified, governs herbalists, general traditional healers, chiropractic professionals, homoeopaths, osteopaths and naturopaths in South Africa (Ahpcsa.co.za., 2024). “The National Department of Health” developed the “National Reference Centre for Traditional Medicines” to implement the National Drug Policy about traditional medicines. The “Drug Policy” part of the “Government’s Reconstruction and Development Programmed” includes traditional medicines. The objectives of the “Department of Pharmacology’s Traditional Medicines Programmed” aim to encourage the usage of high-quality, safe and effective vital traditional medicines; to encourage documentation and scientific verification of traditional medicines; contribute to main health care through offering proper data for traditional healers as well as other medical professionals; and to promote the growth of industry in this sector (WHO, 2002).
Regulations for CAM in Saudi Arabia
Various models have been implemented around the world to govern complementary and traditional medicine medical professions. Prototypes of direct state legalization, governmental authorized self-regulation and autonomous self-regulation” are among them. At the national level, Saudi Arabia has enacted the direct state legalization paradigm. The Ministry of Health (MOH) of Saudi Arabia oversees the National Centre for Complementary and Alternative Medicine (NCCAM). The NCCAM was created by the “Saudi Council of Ministers” via “Resolution 236 (dated 11/8/2008)”. NCCAM is the Saudi official norm for all complementary medicine initiatives; it is closely tied to the Saudi health minister and has a specialist advisory board. Five complementary medical techniques are currently regulated and licensed in Saudi Arabia: cupping treatment, naturopathy, osteopathy, chiropractic and acupuncture. Furthermore, the “Saudi Food and Drug Authority” regulates food supplement items, complementary medicine devices and botanicals (Aboushanabet al., 2019).
REGULATORY STANDARDS AND MARKET APPROVALS FOR HERBAL MEDICINAL PRODUCTS IN INDIA, UNITED STATES AND EUROPEAN UNION
According to the survey results, manufacturers of herbal medicines have a lot of concerns about inconsistent regulatory standards and the ensuing delays in the application submission and approval procedure. To comprehend the variations in approval processes and submission requirements, relative research of drug certification standards for nations including the European nations, India and the United States was carried out. Because they have a long history of use in India, traditional herbal treatments like Unani, Ayurveda and Siddha, are regarded as risk-free. According to the “Drugs and Cosmetics Act of 1940 (DCA)”, neither safety nor efficacy studies are necessary to approve a product for marketing.
Manufacturing and marketing approvals are subject to regulation by the “State Food and Drug Administration (SFDA)”. Under the “Dietary Supplement Health and Education Act of 1994”, the majority of Indian herbal medicines are sold in the United States as dietary supplements. For marketing approval, the Act does not mandate the submission of any efficacy or safety information. Since it is up to the makers to prove the safety of the products, no health claims directed at a specific illness or ailment are permitted. Before creating or marketing dietary supplements, manufacturers are not required to file their goods with USFDA or obtain permission. Any dangerous dietary supplement product must be dealt with by the FDA when it enters the market. According to the survey’s findings, there is a correlation between the highest transmit to the United States and the laxer regulations on dietary supplements. Since no scientific justification is needed, Indian manufacturers opt to market their goods as nutritive or dietary supplements lacking any health claims.
However, in the European Union (EU), preclinical safety data and bibliographic proof are required for applications for marketing permission for traditional medical products. According to “Article 8 (3) (a) to (h), (j) and (k)” of the Traditional Herbal Medicinal Product Directive (2004/24/EC), the applicant must provide qualitative and quantitative details of the therapeutic product’s constituents, an interpretation of the manufacturing process, healing signs, discrepancies, detrimental reactions, form, posology and route of administration to obtain traditional use registration. According to “Article 11 (4)” of “Directive 2001/83/EC”, the application must also include a summary of the product’s features without any clinical information.
Many non-EU items that have not yet been utilized in the EU would be prohibited under Directive 2004/24/EC since a minimal 15 years of EU marketing experience is necessary. In such cases, herbal medications would only be allowed if they could fortunately complete a full course, which calls for safety and efficacy data. For the majority of Indian herbal medicine producers, this is probably going to be very expensive. Additionally, there is a chance that herbal items, which need to be seen as dietary supplements, will end up being classified as herbal medicines. Complex formulations with high concentrations of nutrients will be prohibited and certain herbal product combinations may be restrained. Moreover, the candidate applying must present the quality, limits and records for each mineral and vitamin in addition to the requirements for herbal substances and herbal preparations. This comes at a very hefty price.
Therefore, even though demand for conventional Indian herbal remedies is rising in both regions, the EU’s strict regulatory standards made the US a greater desirable export target than the EU. However, because they are marketed as an add-on rather than medications, Indian traditional herbal treatments do not receive the credit they deserve. Additionally, compared to Indian standards, other nations have their requirements. A common differentiation of pharmacopeia grades indicates diversity in plant-particular factors and standard requirements, including allowable levels for pesticides, heavy metals and microbiological contamination in various nations. Regional and national guidelines have been developed, but only some of them have been adopted. For Indian producers and traders, adhering to so many norms has become a top concern (Sahooet al., 2013).
CONCLUSION
CAM, or complementary and alternative medicine, refers to a wide range of treatment modalities and procedures to foster holistic well-being and address medical issues without the use of traditional medical procedures. Although CAM therapies have grown in popularity and are frequently sought by people looking for alternative healthcare options, it’s important to approach them from a balanced standpoint. For ages, people have adopted natural remedies to relieve the symptoms of depressive disorders and anxiety. Alternatives to prescription high-cost pharmaceuticals and technology advancement can be applied, such as lifestyle changes, dietary changes, supplement treatment and behavioral medication. To ensure that CAM therapies are properly and successfully integrated into the current healthcare delivery system, healthcare administrators and providers need to have a thorough understanding of these therapies. An open discussion between practitioners regarding traditional as well as CAM modalities can result in a more thorough and patient-focused approach to healthcare as the field of healthcare develops, encouraging association and a greater awareness of the potential advantages and disadvantages of CAM.
Cite this article:
Nori LP, Malla J, Vadapalli RR, Bonthagarala B, Dannaram PK, Raju KV. Exploring the Healing Paths: Navigating Complementary and Alternative Medicine. Int. J. Pharm. Investigation. 2025;15(3):313-24.
REFERENCES
- Aboushanab, T., Khalil, M., & Al Ahmari, Y. (2019). The present state of complementary medicine regulation in Saudi Arabia. Journal of Integrative Medicine [Internet], 17(3), 147–149. https://doi.org/10.1016/j.joim.2019.03.010
- MASSAGE magazine. (2008). Acupressure, Breath Awareness Help Diabetes Patients [Internet]. Massage Magazine. Retrieved October 10, 2024, https://www.massagemag.com/acupressure-breath-awareness-help-diabetes-patients-3094/
- Ahpcsa. Retrieved October 10, 2024, co.za. https://ahpcsa.co.za/wp-content/uploads/2015/10/The-Allied-Health-Professions-Act-63-of-1982-_as-amended.pdf
- Ajazuddin, S. S., & Saraf, S. (2012). Legal regulations of complementary and alternative medicines in different countries. Pharmacognosy Reviews [Internet], 6(12), 154–160. https://doi.org/10.4103/0973-7847.99950
- Akter, S., Nazmul Hasan, M., Rokeya, B., Akhter, H., Shamim Gazi, M., Sabrin, F., & Soo Kim, S. (2021). Alternative medicine: A recent overview. In M. Akram (Ed.), Alternative medicine- update. Intech open. IntechOpen. https://doi.org/10.5772/intechopen.97039
- Anderson, R. J., Freedland, K. E., Clouse, R. E., & Lustman, P. J. (2001). The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care [Internet], 24(6), 1069–1078. https://doi.org/10.2337/diacare.24.6.1069
- Batke, P. Google Books: Google book search and its critics. Morrisville, NC. Lulu.com. (2011).
- Brinkley, T. E., Lovato, J. F., Arnold, A. M., Furberg, C. D., Kuller, L. H., Burke, G. L., Nahin, R. L., Lopez, O. L., Yasar, S., Williamson, J. D., & Ginkgo Evaluation of Memory (GEM) Study Investigators. (2010). Effect of Ginkgo biloba on blood pressure and incidence of hypertension in elderly men and women. American Journal of Hypertension [Internet], 23(5), 528–533. https://doi.org/10.1038/ajh.2010.14
- Heart disease facts. (2023) [Internet]. Cdc.gov. Centres for Disease Control and Prevention. Retrieved October 10, 2024, https://www.cdc.gov/heartdisease/facts.html
- Chen, D., Gong, D., & Zhai, Y. (1994). Clinical and experimental studies in treating diabetes mellitus by acupuncture. Journal of Traditional Chinese Medicine, 14(3), 163–166.
- Chen, K.-J., Hui, K. K., Lee, M. S., & Xu, H. (2012). The potential benefit of complementary/alternative medicine in cardiovascular diseases. Evidence-Based Complementary and Alternative Medicine: eCAM [Internet], 2012, Article 125029. https://doi.org/10.1155/2012/125029
- Chow, S. L., Bozkurt, B., Baker, W. L., Bleske, B. E., Breathett, K., Fonarow, G. C., Greenberg, B., Khazanie, P., Leclerc, J., Morris, A. A., Reza, N., Yancy, C. W., & American Heart Association Clinical Pharmacology Committee and Heart Failure and Transplantation Committee of the Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Council on Cardiovascular and Stroke Nursing. (2023). Complementary and alternative medicines in the management of heart failure: A scientific statement from the American Heart Association. Circulation [Internet], 147(2), e4–e30. https://doi.org/10.1161/CIR.0000000000001110
- Clinic C. What do “complementary” and “alternative” medicine really mean? [Internet]. (2023). Cleveland Clinic. Retrieved October 10, 2024, https://my.clevelandclinic.org/health/treatments/17106-wellness–holistic-therapies
- Darnton-Hill, I., Caterson, I., & Colagiuri, S. (2011). Nutrition and the benefits of early interventions in diabetes, cardiovascular and noncommunicable diseases. In J. K. Gerald, R. R. Watson, V. R. Preedy (Eds.), (pp. 365–390). Humana Press. https://doi.org/10.1007/978-1-60761-308-4_23
- de Lima Pimentel, R., Duque, A. P., Moreira, B. R., & Rodrigues, L. F. J. (2019). Acupuncture for the treatment of cardiovascular diseases: A systematic review. Journal of Acupuncture and Meridian Studies [Internet], 12(2), 43–51. https://doi.org/10.1016/j.jams.2018.07.005
- de Valk, H. W. (1999). Magnesium in diabetes mellitus. The Netherlands Journal of Medicine, 54(4), 139–146). https://doi.org/10.1016/s0300-2977(99)00005-4
- Management Board members, Executive Director, Operational Management. (2017). Dietary Reference Values for nutrients Summary report [Internet]. European Food Safety Authority. Retrieved October 10, 2024, https://www.efsa.europa.eu/en/supporting/pub/e15121
- Ellwood, J. (2003). Exploring the benefits of aromatherapy: A case study. Nursing and Residential Care [Internet], 5(10), 474–477. https://doi.org/10.12968/nrec.2003.5.10.11731
- Elson, D. F. MM, & Meredith, M. (1998). Therapy for type 2 diabetes mellitus. WMJ, 97(3), 49–54.
- Ernst, E. (2000). ABC of complementary medicine. Focus on Alternative and Complementary Therapies [Internet], 5(3), 231–231. https://doi.org/10.1111/j.2042-7166.2000.tb02553.x
- Fda.gov. Retrieved October 10, 2024, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/complementary-and-alternative-medicine-products-and-their-regulation-food-and-drug-administration
- Dietary supplement ingredient directory [Internet]. Fda.gov. Retrieved October 10, 2024, https://www.fda.gov/food/dietary-supplements/dietary-supplement-ingredient-directory
- Frishman. (2009).pdf. Retrieved October 10, 2024, http://frishman2009.pdf
- Goodman and Gilman’s the Pharmacological Basis of Therapeutics. Mhprofessional.com (13th ed.) [Internet]. Retrieved October 10, 2024, https://www.mhprofessional.com/goodman-and-gilman-s-the-pharmacological-basis-of-therapeutics-13th-edition-9781259584749-usa
- Gov.in. Retrieved October 10, 2024, https://main.mohfw.gov.in/documents/publication
- Grant, S. J., Bin, Y. S., Kiat, H., & Chang, D. H.-T. (2012). The use of complementary and alternative medicine by people with cardiovascular disease: A systematic review. BMC Public Health [Internet], 12(1), 299. https://doi.org/10.1186/1471-2458-12-299
- Gupta, N., Khera, S., Vempati, R. P., Sharma, R., & Bijlani, R. L. (2006). Effect of yoga-based lifestyle intervention on state and trait anxiety. Indian Journal of Physiology and Pharmacology, 50(1), 41–47.
- Halim, E. M. (2003). Lowering of blood sugar by water extract of Azadirachta indica and Abroma augusta in diabetes rats. Indian Journal of Experimental Biology, 41(6), 636–640.
- Innes, K. E., Bourguignon, C., & Taylor, A. G. (2005). Risk indices associated with the insulin resistance syndrome, cardiovascular disease and possible protection with yoga: A systematic review. The Journal of the American Board of Family Practice [Internet], 18(6), 491–519. https://doi.org/10.3122/jabfm.18.6.491
- Karunanayake, E. H., Jeevathayaparan, S., & Tennekoon, K. H. (1990). Effect of Momordica charantia fruit juice on streptozotocin-induced diabetes in rats. Journal of Ethnopharmacology [Internet], 30(2), 199–204. https://doi.org/10.1016/0378-8741(90)90008-h
- Khosla, P., Gupta, D. D., & Nagpal, R. K. (1995). Effect of Trigonella foenum graecum (Fenugreek) on blood glucose in normal and diabetic rats. Indian Journal of Physiology and Pharmacology, 39(2), 173–174.
- Lawless, J. (2014). Aromatherapy and the mind. Thorsons.
- Madar, Z., Abel, R., Samish, S., & Arad, J. (1988). Glucose-lowering effect of fenugreek in non-insulin dependent diabetics. European Journal of Clinical Nutrition, 42(1), 51–54.
- Malhotra, V., Singh, S., Tandon, O. P., Madhu, S. V., Prasad, A., & Sharma, S. B. (2002). Effect of Yoga asanas on nerve conduction in type 2 diabetes. Indian Journal of Physiology and Pharmacology, 46(3), 298–306.
- Mandal, A. (2014). Cardiovascular drugs [Internet]. News-Medical. Retrieved October 10, 2024, https://www.news-medical.net/health/Cardiovascular-Drugs.aspx
- McGinnis, R. A., McGrady, A., Cox, S. A., & Grower-Dowling, K. A. (2005). Biofeedback-assisted relaxation in type 2 diabetes. Diabetes Care [Internet], 28(9), 2145–2149. https://doi.org/10.2337/diacare.28.9.2145
- Mental health treatments [Internet]. Mental Health America. Retrieved October 10, 2024, https://mhanational.org/mental-health-treatments
- Mladenka, P., Hrdina, R., Bobrovová, Z., Semecky, V., Vávrová, J., Holecková, M., Palicka, V., Mazurová, Y., & Nachtigal, P. (2009). Cardiac biomarkers in a model of acute catecholamine cardiotoxicity. Human and Experimental Toxicology [Internet], 28(10), 631–640. https://doi.org/10.1177/0960327109350665
- Mooradian, A. D., Failla, M., Hoogwerf, B., Maryniuk, M., & Wylie-Rosett, J. (1994). Selected vitamins and minerals in diabetes. Diabetes Care [Internet], 17(5), 464–479. https://doi.org/10.2337/diacare.17.5.464
- Exploring aromatherapy [Internet]. Naha.org. Retrieved October 10, 2024, https://naha.org/explore-aromatherapy/regulations/
- Nahas, R. (2008). Complementary and alternative medicine approaches to blood pressure reduction: An evidence-based review. Canadian Family Physician Medecin de Famille Canadien, 54(11), 1529–1533.
- NCCIH [Internet]. NCCIH. Retrieved October 10, 2024, https://www.nccih.nih.gov/
- Ong, H. T., & Cheah, J. S. (2008). Statin alternatives or just placebo: An objective review of omega-3, red yeast rice and garlic in cardiovascular therapeutics. Chinese Medical Journal [Internet], 121(16), 1588–1594. https://doi.org/10.1097/00029330-200808020-00017
- Pros and cons of mental health medications [Internet]. (2023). Online psychiatrists and TMS therapy | Neuro Wellness Spa. Retrieved October 10, 2024, https://neurowellnessspa.com/pros-and-cons-of-mental-health-medications/
- Org.uk. Retrieved October 10, 2024, https://www.mind.org.uk/
- Polidori, M. C., Mecocci, P., Stahl, W., Parente, B., Cecchetti, R., Cherubini, A., Cao, P., Sies, H., & Senin, U. (2000). Plasma levels of lipophilic antioxidants in very old patients with type 2 diabetes. Diabetes/Metabolism Research and Reviews [Internet], 16(1), 15–19. https://doi.org/10.1002/(sici)1520-7560(200001/02)16:1<15: aid-dmrr71>3.0.co;2-b
- What is mental illness? [Internet]. Psychiatry.org. Retrieved October 10, 2024, https://www.psychiatry.org/patients-families/what-is-mental-illness
- Qidwai, W., Yeoh, P. N., Inem, V., Nanji, K., & Ashfaq, T. (2013). Role of complementary and alternative medicine in cardiovascular diseases. Evidence-Based Complementary and Alternative Medicine: eCAM [Internet], 2013, Article 142898. https://doi.org/10.1155/2013/142898
- Rastogi, S., Pandey, M. M., & Rawat, A. K. S. (2016). Traditional herbs: A remedy for cardiovascular disorders. Phytomedicine [Internet], 23(11), 1082–1089. https://doi.org/10.1016/j.phymed.2015.10.012
- Rathore, S. S., Curtis, J. P., Wang, Y., Bristow, M. R., & Krumholz, H. M. (2003). Association of serum digoxin concentration and outcomes in patients with heart failure. JAMA [Internet], 289(7), 871–878. https://doi.org/10.1001/jama.289.7.871
- Rizos, E. C., Ntzani, E. E., Bika, E., Kostapanos, M. S., & Elisaf, M. S. (2012). Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: A systematic review and meta-analysis. JAMA [Internet], 308(10), 1024–1033. https://doi.org/10.1001/2012.jama.11374
- Sahay, B. K. (2007). Role of yoga in diabetes. The Journal of the Association of Physicians of India, 55, 121–126.
- Sahoo, N., & Manchikanti, P. (2013). Herbal drug regulation and commercialization: An Indian industry perspective. Journal of Alternative and Complementary Medicine [Internet], 19(12), 957–963. https://doi.org/10.1089/acm.2012.0275
- Satyanarayana, M. K., Narayana, R. D., Krishna, R. D., & Gopalakrishna, M. L. B. (1978). A preliminary study on hypoglycaemic and antihyperglycaemic effects of Azadirachta indica. Indian Journal of Pharmacology, 10(3), 247.
- Shaito, A., Thuan, D. T. B., Phu, H. T., Nguyen, T. H. D., Hasan, H., Halabi, S., Abdelhady, S., Nasrallah, G. K., Eid, A. H., & Pintus, G. (2020). Herbal medicine for cardiovascular diseases: Efficacy, mechanisms and safety. Frontiers in Pharmacology [Internet], 11, 422. https://doi.org/10.3389/fphar.2020.00422
- Sibbritt, D., Kaye, M., Millbank, J., Stuhmcke, A., Wardle, J., & Karpin, I. (2018). How are complementary health professions regulated in Australia? An examination of complementary health professions in the national registration and accreditation scheme [Internet]. Complementary Therapies in Medicine, 37, 6–12. https://doi.org/10.1016/j.ctim.2017.12.012
- Stuber, M., Hilber, S. D., Mintzer, L. L., Castaneda, M., Glover, D., & Zeltzer, L. (2009). Laughter, humor and pain perception in children: A pilot study. Evidence-Based Complementary and Alternative Medicine: eCAM [Internet], 6(2), 271–276. https://doi.org/10.1093/ecam/nem097
- Sullivan, S. G., Paolacci, S., Kiani, A. K., & Bertelli, M. (2020). Chiropractic care for hypertension: Review of the literature and study of biological and genetic bases. Acta Bio-Medica: Atenei Parmensis [Internet], 91(13–S), Article e2020017. https://doi.org/10.23750/abm.v91i13-S.10524
- Suzuki, N. (2004). Complementary and alternative medicine: A Japanese perspective. Evidence-Based Complementary and Alternative Medicine: eCAM [Internet], 1(2), 113–118. https://doi.org/10.1093/ecam/neh029
- Takeda, M., Hashimoto, R., Kudo, T., Okochi, M., Tagami, S., Morihara, T., Sadick, G., & Tanaka, T. (2010). Laughter and humor as complementary and alternative medicines for dementia patients. BMC Complementary and Alternative Medicine [Internet], 10(1), 28. https://doi.org/10.1186/1472-6882-10-28
- Mind-body therapies [Internet]. Taking Charge of Your Wellbeing. Retrieved October 10, 2024, https://www.takingcharge.csh.umn.edu/explore-healing-practices/what-are-mind-body-therapies
- Traditional medicine: Its contribution to human health development in the new century: Report of an international symposium. WHO Centre for Health Development (Kobe, Japan). (2000). World Health Organization.
- Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Anderson, C. A. M., Arora, P., Avery, C. L., Baker-Smith, C. M., Beaton, A. Z., Boehme, A. K., Buxton, A. E., Commodore-Mensah, Y., Elkind, M. S. V., Evenson, K. R., Eze-Nliam, C., Fugar, S., Generoso, G., Heard, D. G., Hiremath, S., Ho, J. E., American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2023). Heart disease and Stroke Statistics-2023 Update: A Report from the American Heart Association [Internet]. Circulation. Northwestern.eduCirculation. Retrieved October 10, 2024, https://www.scholars.northwestern.edu/en/publications/heart-disease-and-stroke-statistics-2023-update-a-report-from-the, 147(8), e93–e621. https://doi.org/10.1161/CIR.0000000000001123
- Wallerath, T., Poleo, D., Li, H., & Förstermann, U. (2003). Red wine increases the expression of human endothelial nitric oxide synthase: A mechanism that may contribute to its beneficial cardiovascular effects. Journal of the American College of Cardiology [Internet], 41(3), 471–478. https://doi.org/10.1016/s0735-1097(02)02826-7
- Watts, M. Diabetes medication side effects. Diabetes.co.Uk. (2019).
- Heart attack medicines: What to know about side effects [Internet]. WebMD. Retrieved October 10, 2024, https://www.webmd.com/heart-disease/heart-attack-meds
- Cardiovascular diseases (CVDs) [Internet]. Who.int. Retrieved October 10, 2024, https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- Diabetes [Internet]. Who.int. Retrieved October 10, 2024, https://www.who.int/news-room/fact-sheets/detail/diabetes
- Who.int. Retrieved October 10, 2024, https://apps.who.int/iris/bitstream/handle/10665/42452/WHO_EDM_TRM_2001.2_eng.pdf
- World Health Organization. (2002). Regulatory situation of herbal medicines: A worldwide review. World Health Organization.
- Zhang, X. (2000). Integration of traditional and complementary medicine into national health care systems. Journal of Manipulative and Physiological Therapeutics [Internet], 23(2), 139–140. https://doi.org/10.1016/s0161-4754(00)90085-x.

