ABSTRACT
Background
The present study aims to develop an Elementary Osmotic tablet (EOP) of Rivastigmine Hydrogen Tartrate (RHT). EOP consists of a core tablet suitably coated with a polymeric solution, and an orifice drilled on one side of the tablet.
Materials and Methods
The influence of core variables, including sodium chloride (osmogen) concentration and Polyvinyl Pyrrolidine K30 (PVP K30) concentration, have been investigated and optimized by factorial design. The effect of membrane (coating) variables, including polyethylene glycol 400 (PEG 400) amount and percent coating weight gain have been studied. The rivastigmine release of the optimized system has been investigated in various dissolution media, at different stirring rates, at variable pH, and variable osmotic pressure.
Results
It was observed that PEG 400 incorporated in the coating membrane improved drug release. The sodium chloride had a profoundly positive influence, and PVP K30 had a negative influence on the rivastigmine release. The finding reveals that the core tablet containing sodium chloride (50 mg) and PVP K30 (2.5 mg) coated with the solution containing 20% PEG 400 and 5% weight gain was optimized.
Conclusion
The developed EOP provides the RHT release for up to 24 hr with improved bioavailability. The results instigated a controlled release of rivastigmine.
INTRODUCTION
Controlled drug delivery systems are dosage forms that not only delay the release rate but are designed to deliver specific release rates of the drug within a predetermined period.1 An ODD is one such formulation that enables controlled and continuous delivery of the drug, maintaining the concentration of the drug within the therapeutic window. An EOP incorporates an active agent with apt osmotic pressure into a tablet and coated with a semi-permeable membrane, usually of cellulose acetate.2 A small orifice drilled through the coating using Laser or high-speed mechanical drill pumps the drug out of the system at a controlled rate.3
Rivastigmine, a dual inhibitor of cholinesterase, is used in the management of cognitive impairment associated with Parkinson’s disease and Alzheimer’s disease.4 It is initially dosed at 1.5 mg twice daily, further increased by 1.5 mg twice daily for two weeks, and a maximum of 6 mg dose is tolerable twice daily.5 It has a low bioavailability of 36% for a 3 mg dose.6 It is absorbed from the stomach, as well as intestine7 and the presence of food delays the absorption of rivastigmine by 30%.8 It is metabolized by cholinesterase by hydrolysis. Hence exhibits minimal drug-drug interactions.9 Rivastigmine, at high doses, is associated with gastrointestinal adverse events like nausea, tremor, vomiting, and diarrhea.10,11 The adverse events owing to a rapid increase in the maximum concentration of the rivastigmine in the brain, fluctuation in plasma levels, and a shorter time to reach Cmax.8,12 For oral rivastigmine dosage forms, reducing the pharmacokinetic fluctuation may overcome gastrointestinal adverse events and improve tolerability.13,14
Research conducted for rivastigmine includes controlled-release tablets8,15,16 sustained-release tablets,17 microparticles,18 nanoparticles,19–24 buccoadhesive films,14 liposomes25–28 nanostructured lipid carriers29 dry powder inhalation,30 transdermal patch,6,31,32 microporous osmotic tablet.33 However, no study on EOP for RHT was previously reported. Rivastigmine osmotic tablets may have the potential to provide a comparable area under the curve to 1.5 mg BID rivastigmine conventional dose, provide continuous drug delivery, steadier plasma levels, improve bioavailability, and reduce gastrointestinal adverse effects. Rivastigmine hydrogen tartrate, very soluble in water,34 is an exemplary candidate for EOP.35 Once-daily rivastigmine potentially improves treatment compliance and convenience. The present work aims to investigate the influence of core formulation variables such as osmogen concentration and amount of binder; to investigate the influence of membrane variables such as amount of the plasticizer and percentage coating weight gain on drug release; to propose an optimized osmotic formulation; to evaluate the in vitro release of target formulation in various dissolution media, at different agitation rates, pH conditions; to investigate biopharmaceutical parameters in rats.
MATERIALS AND METHODS
Materials
RHT was procured from Dr. Reddy’s Laboratories Ltd., Hyderabad. Sodium chloride, avicel pH 101, talc, PVP K30, PEG 400, hydrochloric acid, sucrose, and sodium acetate were purchased from Merck Specialties Pvt. Ltd., India. Glacial acetic acid, potassium dihydrogen orthophosphate, acetone, magnesium stearate, and sodium hydroxide were acquired from S.D Fine Chemicals, India. Ethanol was purchased from Merck Ltd., India. Orthophosphoric acid was purchased from Rankem Ltd., India.
Experimental animals
The Wistar rats used were housed under a standard environment by the CPCSEA norms and were fasted overnight before treatment. All the animal experiments were accomplished after approval of the protocol by the Institutional Animal Ethics Committee (IAEC) of Jeeva Life Sciences, Shanti Nagar (CPCSEA/ IAEC/JLS/17/0322/053).
Compatibility study
Drug excipient compatibility study was done using Fourier Transform Infrared Spectroscopy (FTIR) and Differential Scanning Calorimetry (DSC).36
FTIR analysis
The FTIR spectra of RHT drug and the optimized formulation were analyzed using Bruker FTIR, Germany (Attenuated Total Reflection, Alpha II) by KBr pellet method37 to detect the compatibility betwixt the pure drug and excipients. The spectra were recorded over the frequency of 4000 cm-1 to 400 cm-1.
DSC analysis
The thermograms of the RHT drug and the optimized formulation were obtained using a DSC (DSC-60, Shimadzu, Japan) to confirm the drug and excipients compatibility study. The samples were heated over 50-300°C (temperature range) at 10°C per minute (heating rate) in the constant nitrogen atmosphere (30 mL/min). The instrument was calibrated with indium (calibration standard, purity >99.9%).38
Preparation of RHT EOP
Preparation of core
The ingredients delineated in Table 1 except magnesium stearate and talc were mixed for 10 min and there by granulated with water. The resulting wet mass was passed through mesh # 20. Granules were dried at 50°C. Finally, dried granules blended with magnesium stearate and talc was compressed into tablets and was evaluated.
| Ingredients (mg) | F1 | F2 | F3 | F4 |
|---|---|---|---|---|
| RHT | 4.8 | 4.8 | 4.8 | 4.8 |
| Sodium chloride | 25 | 50 | 25 | 50 |
| PVP K30 | 2.5 | 2.5 | 5 | 5 |
| Avicel pH 101 | 213 | 188 | 210.5 | 185.5 |
| Magnesium stearate | 2.5 | 2.5 | 2.5 | 2.5 |
| Talc | 2.5 | 2.5 | 2.5 | 2.5 |
Composition of RHT EOP.
Coating of tablets
The solution containing 3 g Cellulose Acetate (CA) dissolved in 100 mL of acetone and ethanol solution (80:20) with various PEG 400 levels was employed for coating. The coating composition is elaborated in Table 2. The coating pan (VJ INSTRUMENTS, India) was operated at 50 rpm beside hot air inlet temperature was kept at 38-42°C39 with a fixed spray rate of 4-5 mL/min.40 The desired weight gain (5%, 7%, and 10%) was obtained by controlling the volume of the coating solution.41 The coated tablets were dried at 50°C in the tray dryer. A mechanical micro drill was employed for drilling an orifice of 0.5 mm.42
| Code | PEG 400 (v/w% of CA) | Percent weight gain (%) |
|---|---|---|
| C1 | 10 | 5 |
| C2 | 10 | 7 |
| C3 | 10 | 10 |
| C4 | 20 | 5 |
| C5 | 20 | 7 |
| C6 | 20 | 10 |
RHT coating composition.
Factorial design of EOP
To investigate the effect of critical core parameters on drug release 22 factorial design was executed. Sodium chloride and PVP K30 were chosen as independent factors whereas percent drug release at 1 hr, 4 hr, 8 hr, and 20 hr were chosen as the dependent factors.
Preformulation characteristics
The prepared blend was appraised for physical characteristics (angle of repose, bulk and tapped density, Carr’s index and Hausner’s ratio to study the flow properties of the powder blend.43
Evaluation of RHT tablets
The osmotic tablets were appraised for physical integrity via weight variation (n=20) using electronic balance (Sartorius, India), thickness (n=6) using Vernier calipers (Mitutoyo, Japan), hardness (n=6) using Monsanto hardness tester (Sisco, India), friability (n=10) using a friabilator (Labindia, India), and drug content (n=6) using a UV-visible spectrophotometer (Labindia, India).
In vitro rivastigmine release
In vitro rivastigmine release from EOP was carried out in 8-station dissolution apparatus (DS 8000, Labindia, India) using the paddle method at 37±0.5°C at 50 rpm in 900 mL of dissolution media. In vitro study was performed in acid (HCl, pH 1.2) for 2 hr, thereafter buffer (phosphate buffer, pH 6.8) up to 24 hr. Subsequently, 5 mL of solution was suitably withdrawn at 0, 1, 2, 4, 6, 8, 10, 12, 16, 18, 20 and 24 hr and there by replaced with the fresh medium. Immediately, the solution was filtered and determined spectrophotometrically.29
Coating membrane morphology
The surface morphology of the osmotic tablet was examined by scanning electron microscope (SEM) JEOL Ltd., Japan. The sample was manually dispersed onto a carbon tab (double adhesive carbon coated tape) adhered to an aluminum stub and then sputter-coated (POLARAON -E 3000) with a thin layer of gold (to good resolution), under vacuum (for better contrast) maintained at 4°C with 30-kV acceleration voltage.44
Dissolution profile modeling
Impact of orifice diameter
The impact of orifice diameter on in vitro rivastigmine release was studied by mechanically drilling various orifices of about 0.4, 0.5, and 0.6 mm on the optimized formulation.43 Subsequently the drilled tablets were subjected to dissolution.
Impact of pH
To study the impact of pH on in vitro rivastigmine release, the dissolution studies of optimized formulation were carried out in HCl, pH 1.2 (0 to 2 hr), acetate buffer pH 4.6 (2 to 4 hr), and phosphate buffer pH 6.8 (4 to 24 hr).
Impact of agitation intensity
To study the impact of agitation intensity on in vitro drug release, the dissolution study of optimized formulation was suitably performed at various agitation conditions of 50, 100, and 150 rpm in the same dissolution medium.
Impact of osmotic pressure
To ensure the mechanism of release follows only osmotic pressure, the dissolution study of optimized formulation was carried out in the media of different osmotic pressures. Graded concentrations of sucrose are added to produce osmotic pressure of 10, 15, and 20 atm in the phosphate buffer pH 6.8.47
Pharmacokinetic analysis
Three groups of six male Wistar rats (230-250 g) were selected. RHT drug suspension and optimized osmotic tablet formulation were administered orally to groups I and II respectively. The marketed formulation (Exelon patch 5) was fixed with its drug-releasing surface adhered to the abdominal skin of group III. Periodically, the plasma samples were collected through retro-orbital plexus at samples at 0, 1, 2, 4, 6, 8, 12, 16, 20, and 24 hr. Blood samples were heparinized and frozen. Plasma was separated by centrifugation using Remi, C24BL centrifuge, and further processed and analyzed by RP-HPLC method.
RP-HPLC for in vivo estimation of RHT
A Simple and efficient RP-HPLC technique was developed to estimate RHT concentration in the rat (Wistar) plasma. All the specifications of the developed method include ODS C18, 250 mm×4.6 mm, 5 μm (particle size), acetonitrile: 0.05 M potassium dihydrogen orthophosphate buffer pH 3.5 (80:20, v/v) as mobile phase, flow rate of 1.3 mL/min. 15 μL was injected in HPLC and detected at 220 nm. For the analysis, a rat plasma sample (200 μL) containing spiking solutions of RHT was deproteinated with 500 μL of acetone, vortexed, there after centrifuged at 12,000 rpm for 5 min. The supernatant was evaporated at 50±2°C, and the residue remained was reconstituted with the mobile phase. It was vortexed, again centrifuged and the supernatant liquid was injected into the HPLC (WATERS, Alliance 2695) system.
Stability study
RESULTS
FTIR analysis
The FTIR peaks of RHT drug were analogous to that specified by Simon A et al. 2016a (3543, 1723, 1696, 1465, 1368 cm–1). Figure 1 illustrates carbamate band at 1723 cm-1. The bands at 3000-2800 cm-1 (3010, 2953, 2923, and 2869) region were assigned to CH3 stretching bands. The spectrum of RHT optimized formulation exhibited similar characteristic peaks which demonstrated no chemical interaction betwixt the drug and excipients.
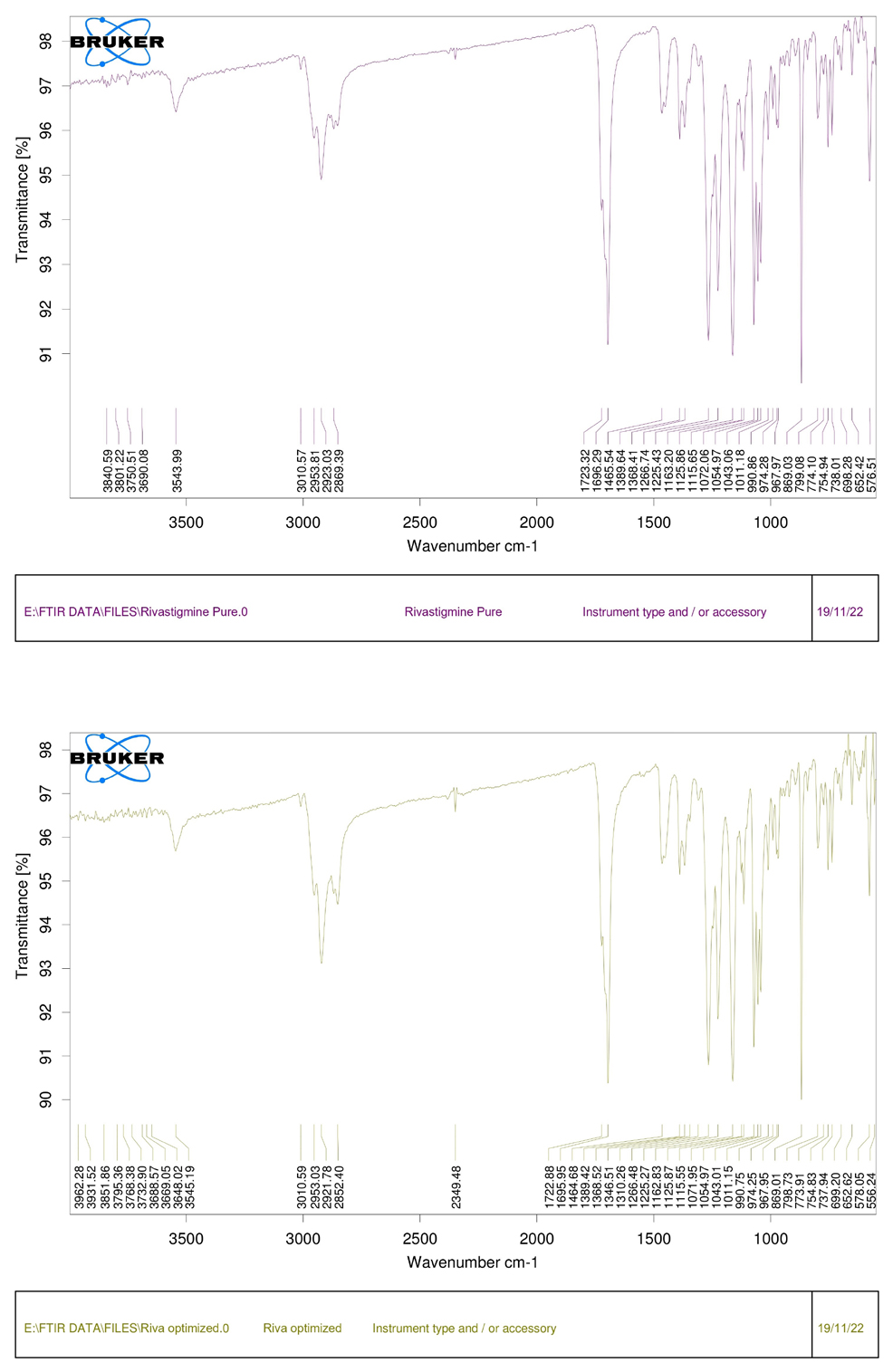
Figure 1.
FTIR spectra of (A) RHT drug, and (B) RHT optimized formulation.
DSC analysis
The DSC thermogram (Figure 3) illustrates a fusion endotherm of 121.3°C (melting point) for RHT pure drug and an endotherm of 118.6°C for RHT optimized formulation. The thermogram of optimized blend well-preserved rivastigmine peak with slight reduction of fusion which demonstrated significant compatibility with other excipients.
Preformulation characteristics
The bulk density and the tapped density of the granules ranged from 0.495 to 0.520 g/mL and 0.581 to 0.608 g/mL respectively. The angle of repose ranged from 24.41° to 26.62°, the Compressibility index ranged from 12.85% to 16.33, and Hausner ratio ranged from 1.16 to 1.22.
Preparation and evaluation of RHT osmotic tablets
The RHT osmotic formulation was developed for controlled release of drug up to 24 hr (once daily dosing). F1 formulation was coated with C1 to C6 formulation for optimizing coating composition. The prepared RHT tablets were evaluated for physical integrity recorded in Table 3.
| Batch | Thickness (mm)* | Hardness (kg/cm2)* | Weight Variation (%)** | Friability (%)* |
|---|---|---|---|---|
| F1 | 3.62±0.229 | 8.45±0.301 | 0.33±0.267 | 0.56±0.22 |
| F2 | 3.55±0.32 | 8.42±0.285 | 0.37±0.286 | 0.48±0.20 |
| F3 | 3.56±0.25 | 8.3±0.109 | 0.38±0.233 | 0.53±0.18 |
| F4 | 3.64±0.25 | 8.3±0.126 | 0.52±0.427 | 0.5±0.24 |
Physical integrity parameters of RHT tablets.
Table 3a: Physical integrity parameters of RHT core tablets.
| Batch | Thickness (mm)* | Hardness (kg/cm2)* | Weight Variation (%)** | Drug content (%)* |
|---|---|---|---|---|
| F1C1 | 4.07±0.052 | 8.45±0.309 | 0.488±0.471 | 98.18±3.91 |
| F1C2 | 4.17±0.045 | 8.42±0.307 | 0.74±0.538 | 98.10±4.06 |
| F1C3 | 4.24±0.025 | 8.29±0.106 | 0.470±0.521 | 94.92±2.70 |
| F1C4 | 4.02±0.132 | 8.30±0.13 | 1.329±0.937 | 98.65±5.27 |
| F1C5 | 4.14±0.033 | 8.30±0.13 | 1.9524±1.117 | 99.12±1.67 |
| F1C6 | 4.27±0.032 | 8.30±0.13 | 0.56±0.241 | 99.75±1.65 |
| F2C4 | 4.275±0.024 | 8.42±0.307 | 0.515±0.401 | 99.58±1.12 |
| F3C4 | 4.183±0.112 | 8.29±0.106 | 0.577±0.391 | 99.63±1.26 |
| F4C4 | 4.066±0.136 | 8.3±0.13 | 1.005±0.855 | 99.04±1.97 |
Physical integrity of RHT coated tablets.
In vitro release of rivastigmine
All batches of RHT osmotic tablets were subjected to dissolution analysis. All F1C1-F1C6 and F1C4 to F4C4 batches showed controlled drug release up to 76% to 91% and 79% to 96% RHT release after 24 hr and the results are graphically presented in Figure 2.
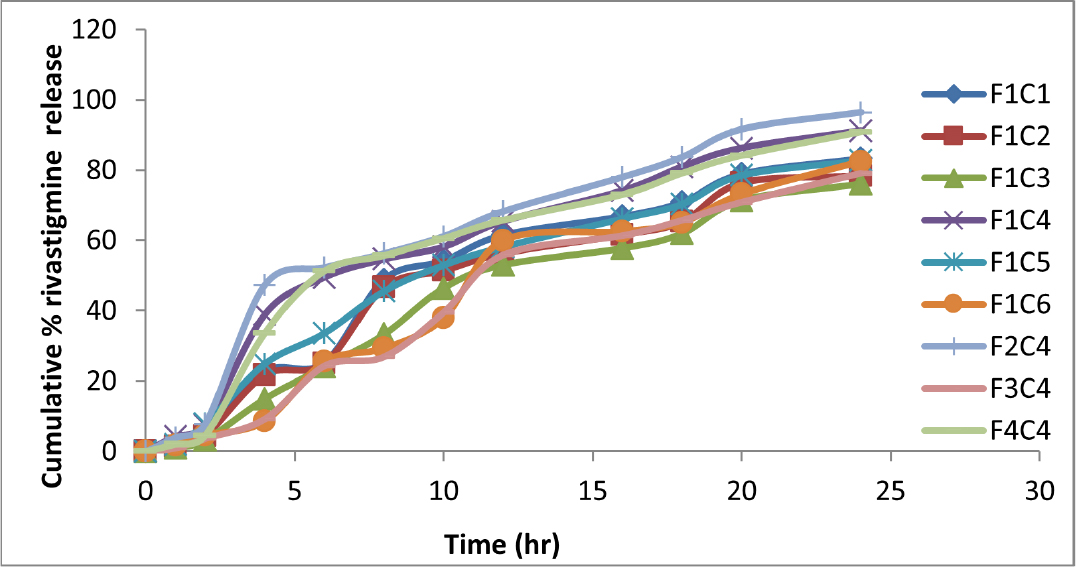
Figure 2.
In vitro dissolution of RHT osmotic tablets.
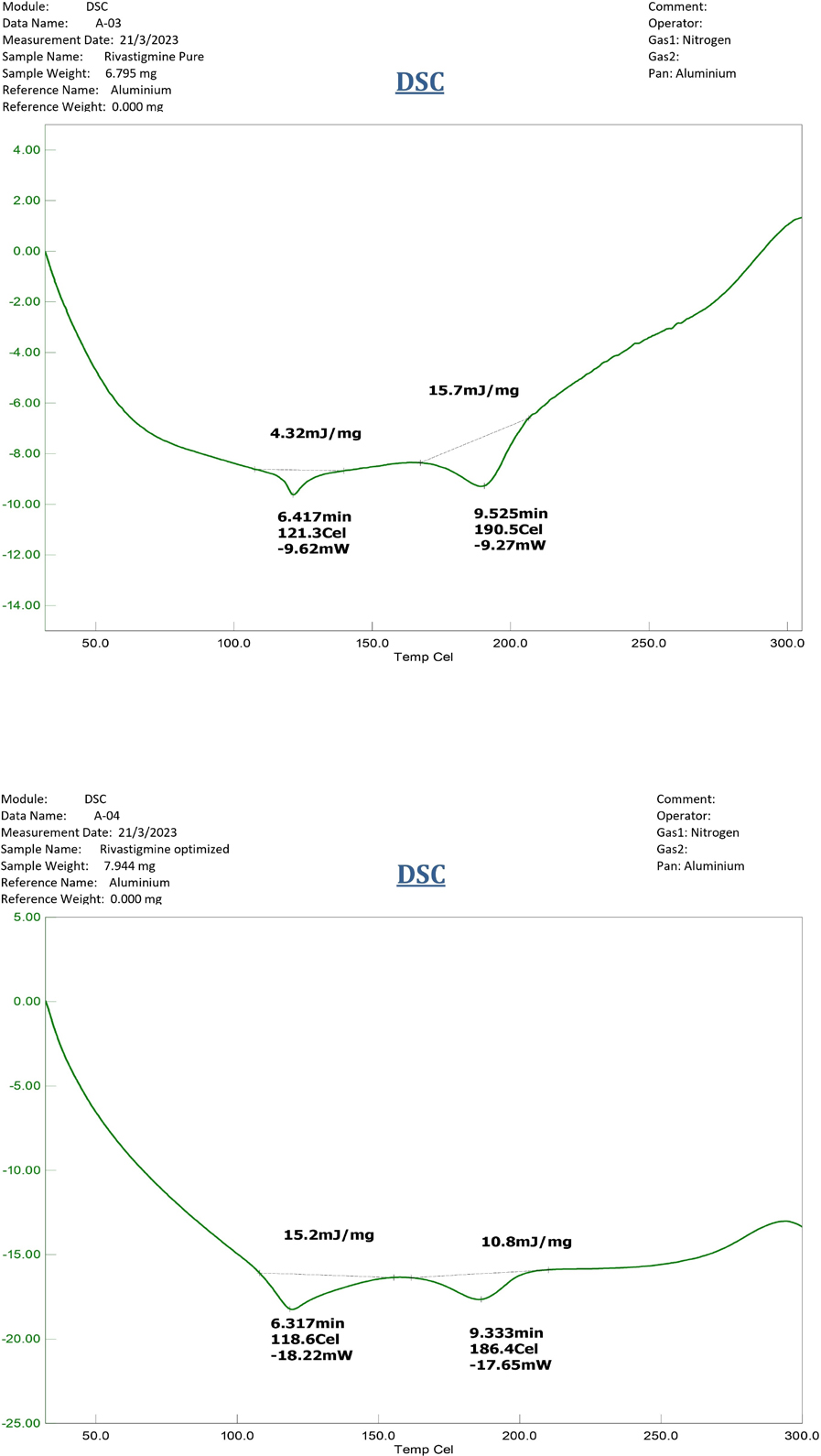
Figure 3.
DSC Thermogram of (A) RHT drug, and (B) RHT optimized formulation.
Impact and optimization of membrane variables
To optimize the membrane variables on drug release, same core tablets (F1 formulation) were coated with coating compositions C1 to C6 (Table 2). Optimizing coating composition involved, analysis similar to specification of in vitro controlled delivery of metoprolol (USP) wherein not more than 25% in 1 hr, between 20% and 40% in 4 hr, between 20% and 40% in 4 hr, between 40% and 60% in 8 hr and not less than 80%.49
Plasticizer level
The influence of PEG 400 level (10%, and 20%v/w of CA) on rivastigmine release from formulations F1C1 and F1C4 are recorded in Figure 4. It was apparent that as the concentration of plasticizer increased, the cumulative rivastigmine release increased because the porosity of the membrane increased with higher permeability of dissolution media.50 PEG 400 at 20%v/w of PEG 400/CA provided a controlling effect on rivastigmine release and was optimized.
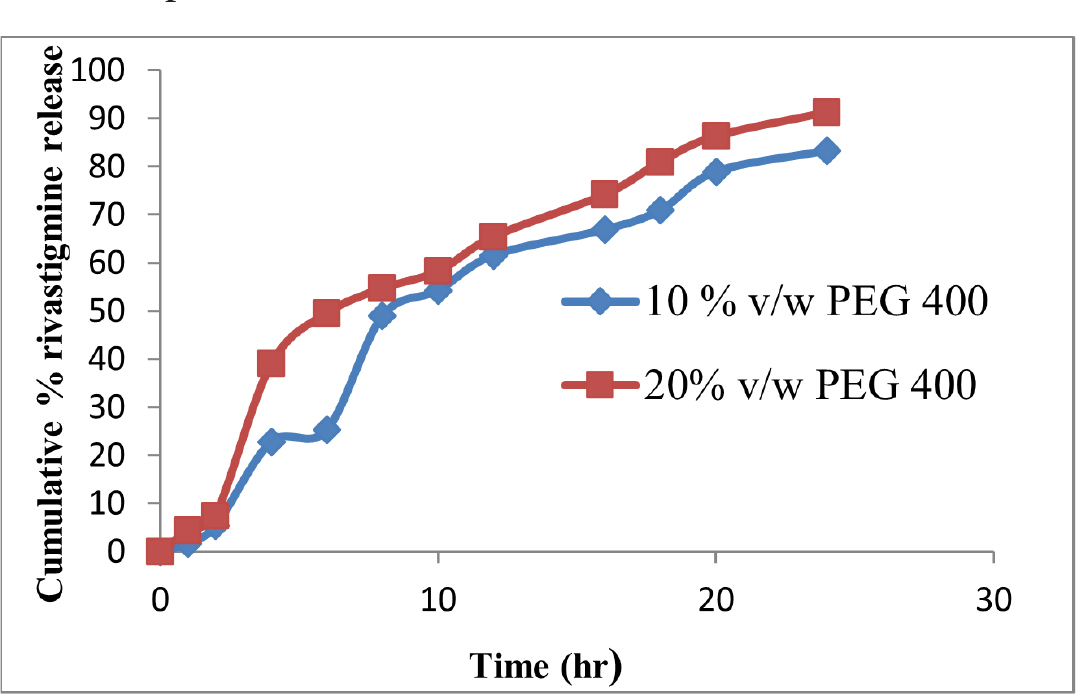
Figure 4.
Dissolution profile at varied plasticizer level.
Percent weight gain
The influence of coating weight gain (5%, 7%, and 10%w/w) on rivastigmine release for formulations F1C4, F1C5, and F1C6 is recorded in Figure 5. It was apparent that as the coating weight gain increased, the cumulative rivastigmine release decreased due to the low ingress of dissolution media.51 The 5% weight gain had a controlling effect on rivastigmine release and was optimized.
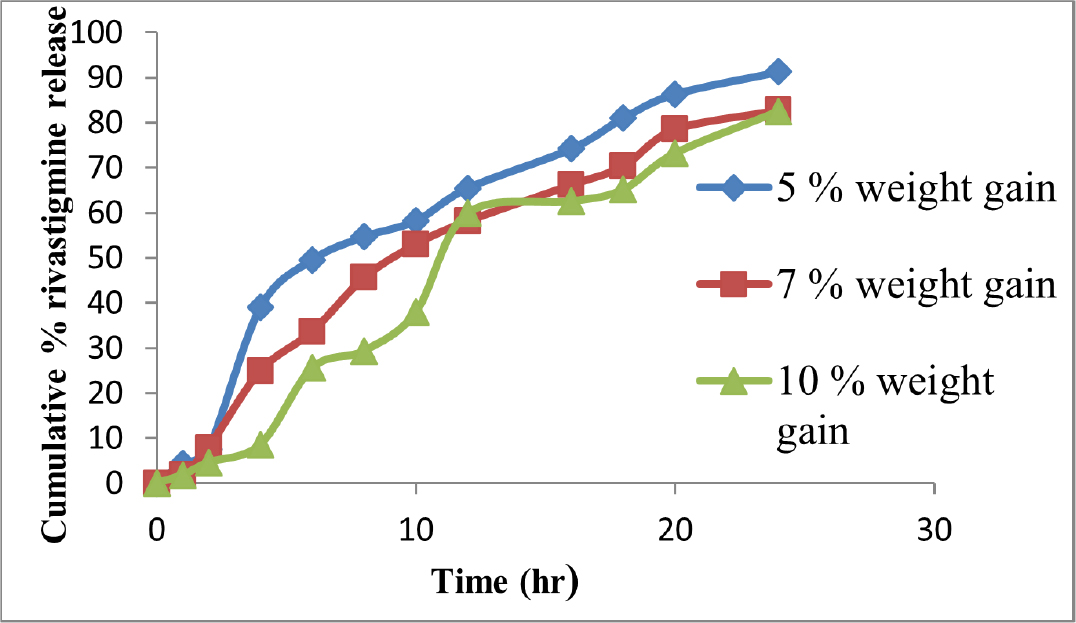
Figure 5.
Dissolution profile at varied coating weight gain.
Experimental design and optimization
The osmotic formulation of RHT was optimized by 22 factorial design using Design-Expert® Software (Stat-Ease Inc., Minneapolis, USA). The regression equations enabled us to know the impact of independent variables on drug responses. The positive and negative mathematical signs of the coefficient of variables implicate that variable and response are directly and indirectly proportional respectively. Contour plots recorded the responses as a function of the independent variable. Response surface plots visualized the relationship betwixt dependent and independent variables. The model was significant for rivastigmine release. The polynomial equations obtained for percent rivastigmine release at 1, 4, 8, and 20 hr are tabulated in Table 4. Figure 6 illustrates contour and response surface graph of rivastigmine release at 1,4,8 and 20 hr.
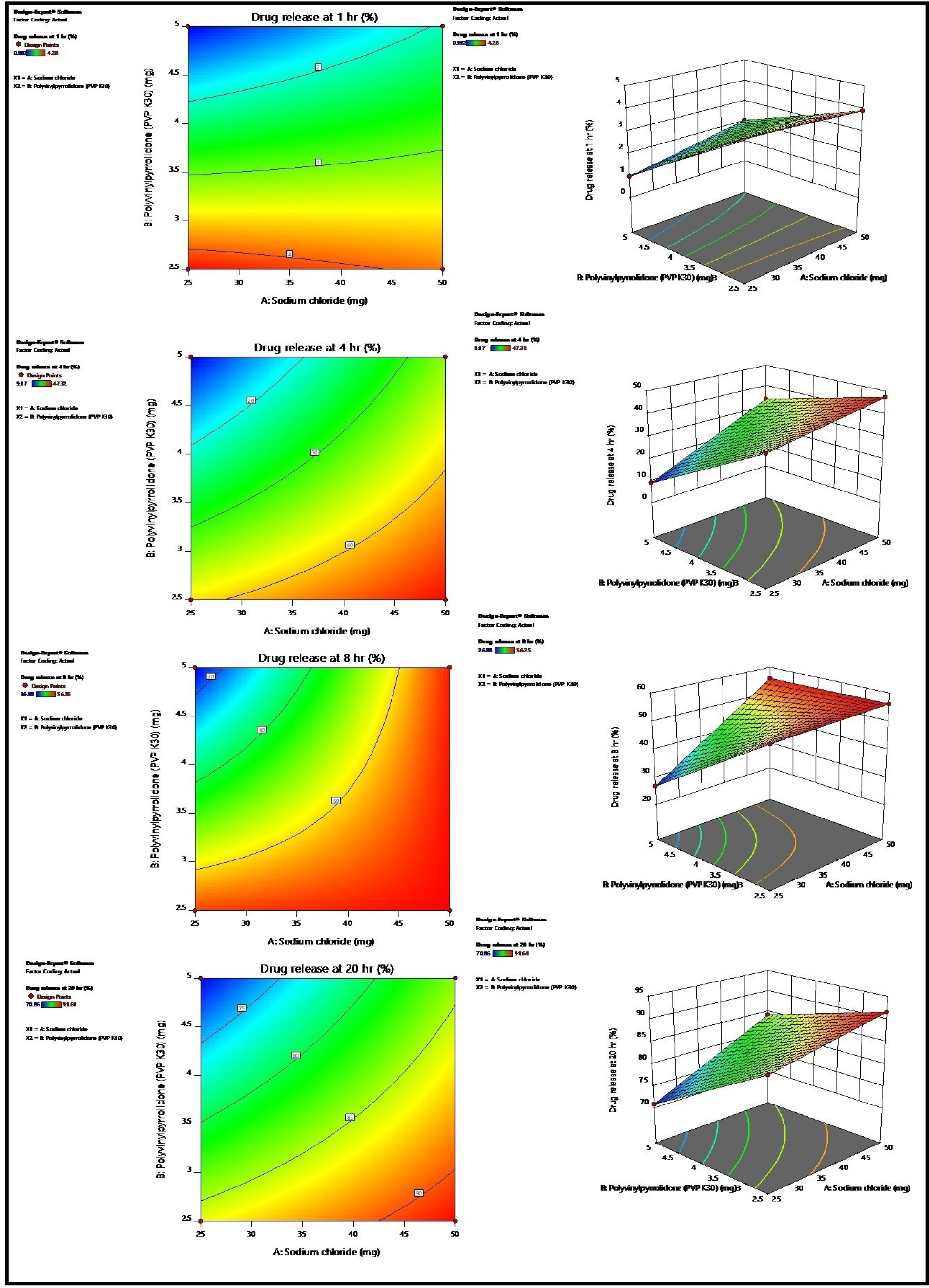
Figure 6.
Percent drug release at [A] 1 hr, [B] 4 hr, [C] 8 hr, and [D] 20 hr (contour plot and response surface graph).
| Response | Polynomial equation |
|---|---|
| Percent drug release at 1 hr. | =+2.81+0.1778*A-1.29*B+0.3577*AB |
| Percent drug release at 4 hr. | =+32.27+8.22*A-10.85*B+4.03*AB |
| Percent drug release at 8 hr. | =+48.37+7.60*A-7.09*B+6.81*AB |
| Percent drug release at 20 hr. | =+83.24+4.66*A-5.71*B+2.00*AB |
The polynomial equation for percent rivastigmine release.
Desirability function-Optimized formulation
A desirability approach was used for selecting optimized formulation. The overlay results instigated that F2C4 formulation with sodium chloride (50 mg) and PVP K30 (2.5 mg) was optimized.
Coating membrane morphology
SEM images of RHT optimized tablets are shown in Figure 7. The intact pore and semi permeable membrane with few pores were visualized.
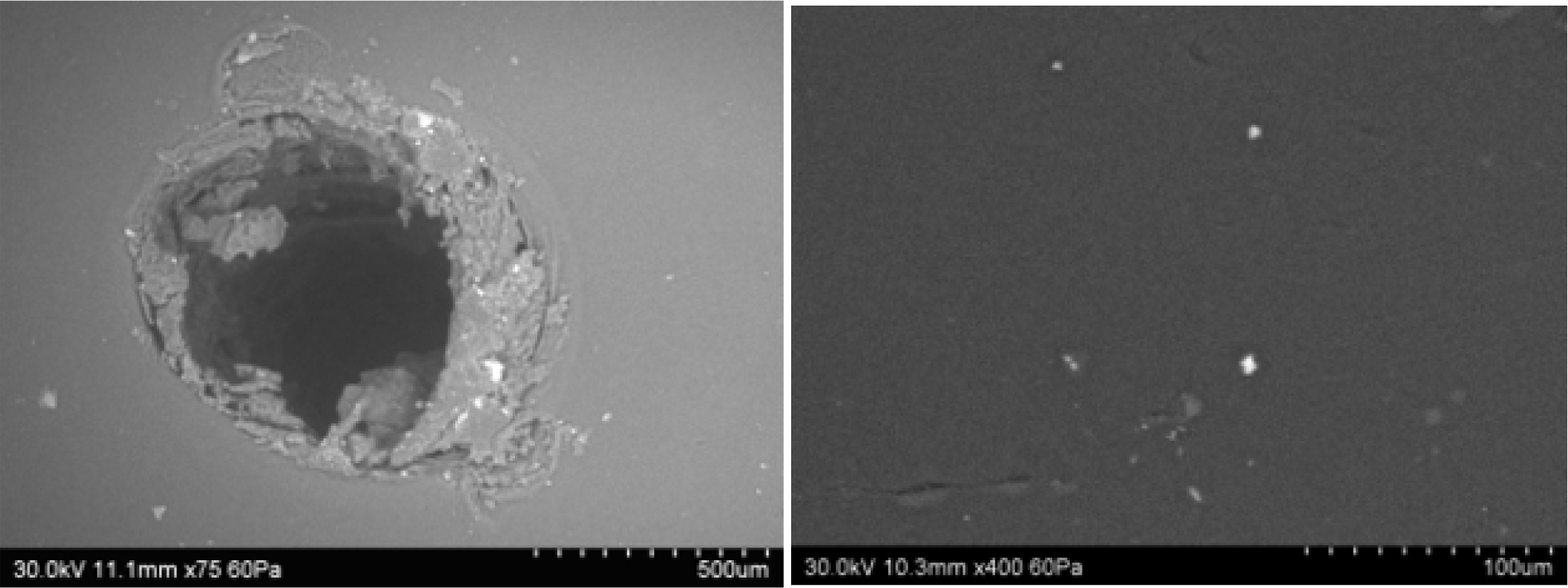
Figure 7.
SEM micrographs of optimized formulation.
Dissolution profile modeling
The regression analysis (R2) for different drug release models is reported in Table 5. All the formulations have shown very close correlation values for zero-order and first-order kinetics. After an initial lag phase of 2 hr, the optimized formulation has shown R2 values of zero-order, first-order, Higuchi, Korsmeyer’s-Peppas and Hixon-Crowell as 0.992, 0.908, 0.980, 0.970, and 0.989. The highest R2 values of zero order confirm the controlled release of RHT.
| Time (day) | Rivastigmine osmotic tablets F2C4 stored at 40°C and 75% RH | |
|---|---|---|
| % Drug Content | % Cumulative drug release (in 24 hr) | |
| 1st day | 99.58±l.l2 | 96.37±0.68 |
| 30th day | 99.58±2.28 | 96.30±0.88 |
| 60th day | 99.54±0.85 | 96.3l±0.56 |
| 90th day | 99.54±l.68 | 96.3l±0.77 |
| 180th day | 99.50±2.05 | 96.25±0.80 |
Stability data of rivastigmine optimized formulation F2C4 at 40°C and 75% RH.
Impact of orifice diameter
The rivastigmine release profiles shown in Figure 8 illustrates that the rivastigmine release from the RHT osmotic tablet was insignificant to orifice diameter.
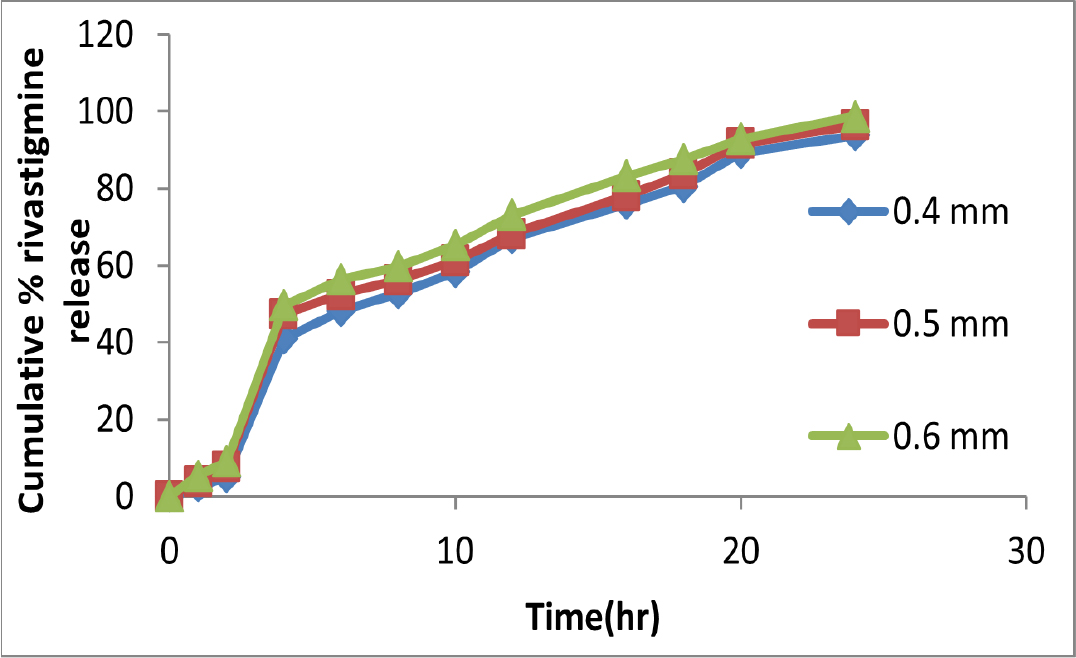
Figure 8.
In vitro rivastigmine release at variable drilling orifice.
Impact of stirring rate
The in vitro rivastigmine release shown in Figure 9 illustrated the release was similar at all agitation speeds, assuring the rivastigmine release was independent of intensity of stirring.
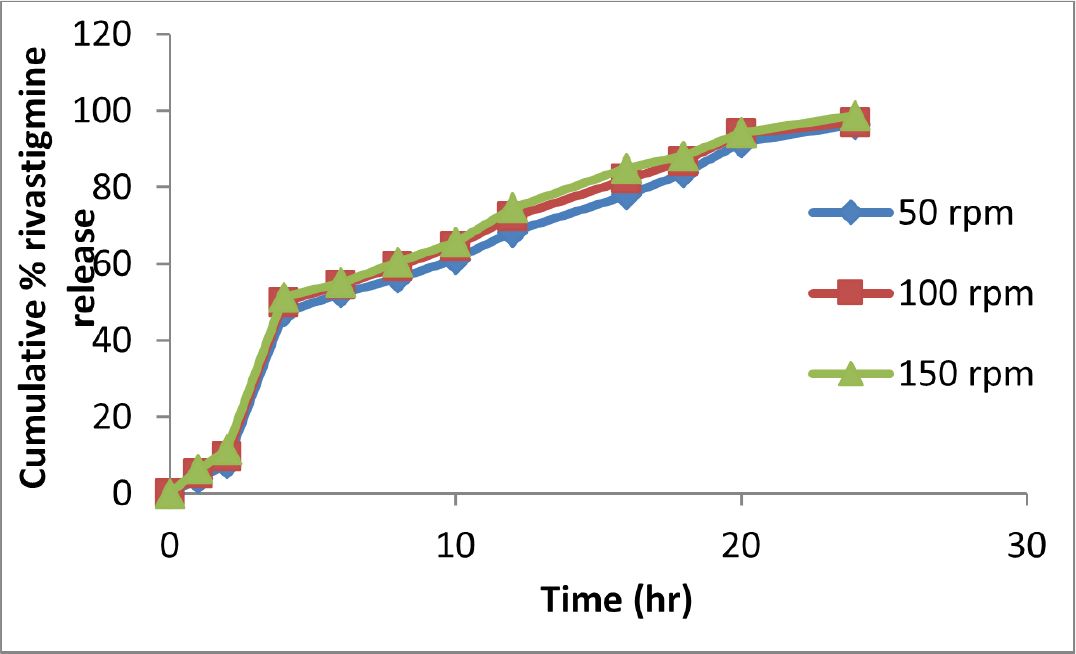
Figure 9.
In vitro release of rivastigmine at variable stirring rate.
Impact of pH of dissolution media
The in vitro rivastigmine release shown in Figure 10 indicated that the release of drug was similar at all pH, assuring the rivastigmine release was independent of pH of dissolution media.
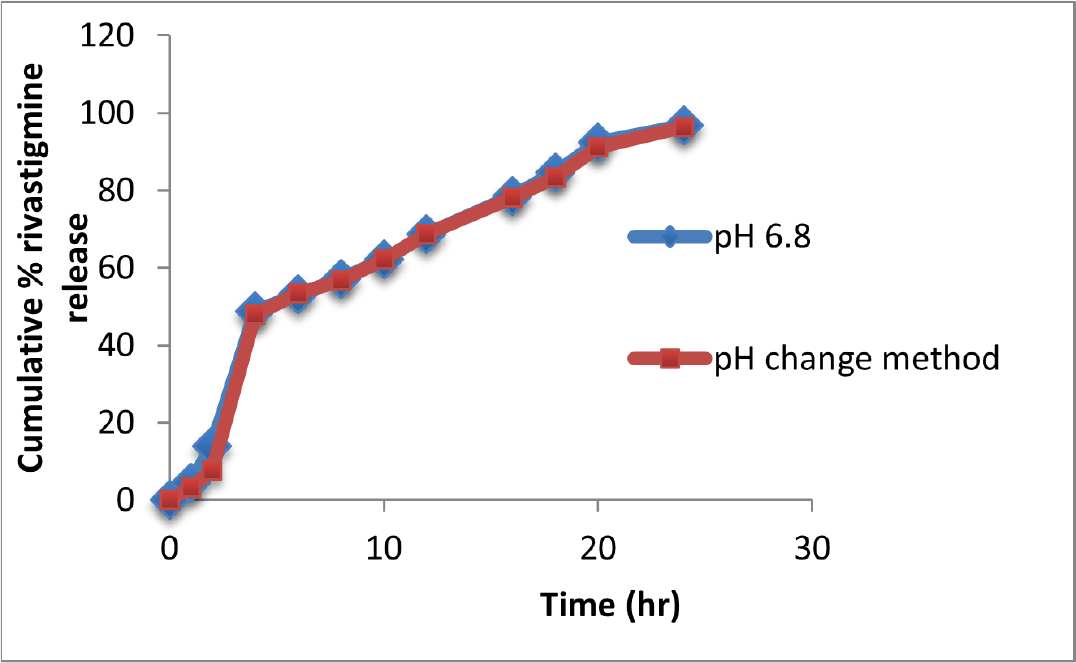
Figure 10.
In vitro rivastigmine release at pH of dissolution media.
Impact of osmotic pressure
The in vitro rivastigmine release shown in Figure 11 indicated that as the osmotic pressure of the medium increased rivastigmine release decreased significantly.
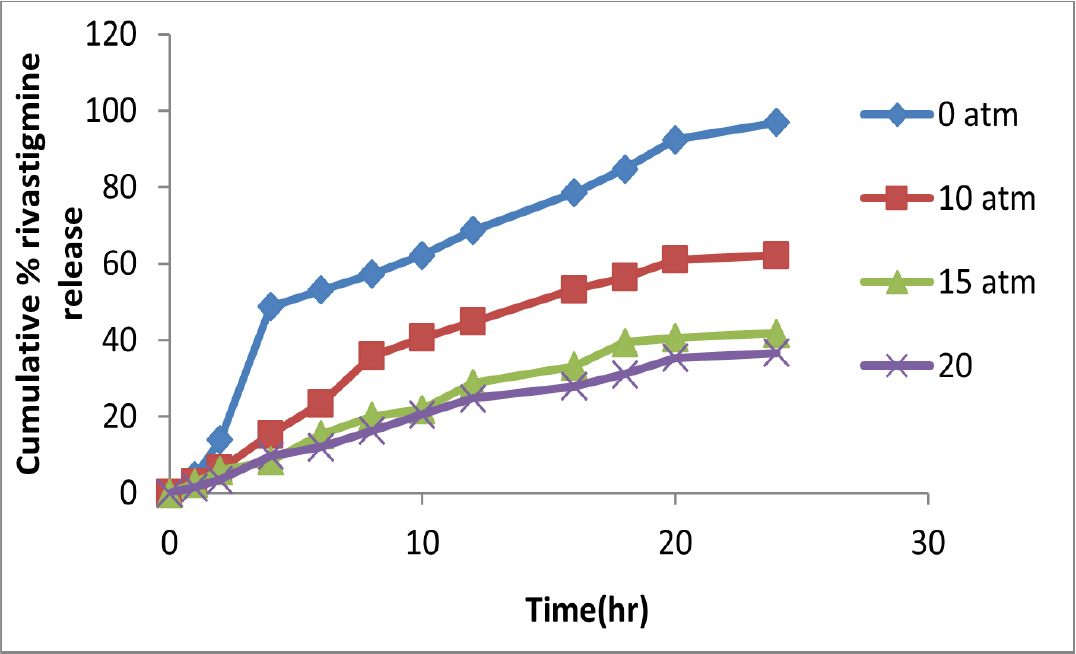
Figure 11.
In vitro rivastigmine release at pH of dissolution media.
A bioanalytical method for rivastigmine estimation
RP-HPLC method was validated and was found suitable for rivastigmine bio-analysis. A good linearity (R2=0.999) for concentration range 250-1250 ng/mL, RSD values lower than 2%, mean recovery rate approximated to 100% was observed. The developed method enabled pharmacokinetic estimations of rivastigmine from rat plasma.
Pharmacokinetic analysis
The pharmacokinetic parameters of rivastigmine drug suspension, optimized osmotic tablet formulation and marketed formulation are shown in Figure 12. It was apparent that rivastigmine osmotic optimized tablet Cmax value occurs at 4 hr and can consistently decline for nearly about 24 hr.
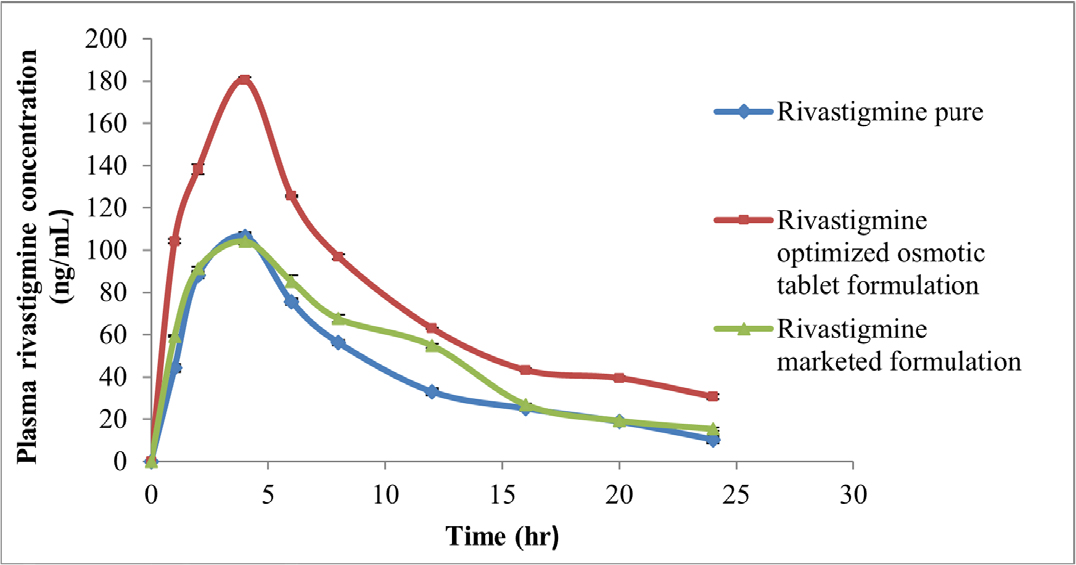
Figure 12.
Mean plasma rivastigmine concentration of RHT suspension, optimized osmotic tablet and marketed formulation.
Stability of the RHT optimized tablet
Data obtained for the RHT optimized tablet stability study is reported in Table 5 which confirmed that the RHT osmotic formulation was stable at storage conditions.
DISCUSSION
The FTIR scans, DSC thermograms of rivastigmine and optimized formulation confirmed compatibility of excipients with RHT. The preformulation characteristics of RHT blend showed that all the batches have good flow properties acceptable for tablet compression. The operational aspects of developed elementary osmotic pump tablets include a core that is surrounded by a rate-controlling semi-permeable coating. The ingress of water into the membrane dissolved the drug enabling release of drug by the phenomenon of osmosis. The F1 formulation was used for optimizing six coating formulations. The coating composition C4 was optimized based on the release profile similar to controlled release specified in literature.49 Also, the effect of membrane variables was studied. Increase in the percent weight gain, decreased the RHT release.42 Increase in the level of PEG 400 increased RHT release because the porosity of the membrane increased as water-soluble plasticizer PEG 400 solubilizes in the dissolution media.39,50
In the factorial design, at all the four time points, the coefficients of A have a positive sign indicating an increase in the concentration of factor A (sodium chloride) increased the drug release and B has a negative sign in the equation indicating an increase in concentration of factor B (PVP K30) decreased the drug release. The positive sign of interaction term AB indicates the interaction of sodium chloride and PVP K30 increased drug release. The positive sign of the interaction term AB indicates interaction of sodium chloride and PVP K30 has a positive effect on drug release. Investigation of critical core formulation variables carried out by factorial design lead to an optimized formulation F2C4 from Design Expert analysis. A good relationship between the practical and predicted values and desirability function of 0.97 indicated the validity and practicability of the model. This indicates that the analysis is significant. As the concentration of sodium chloride increased, the RHT release increased.46 As the concentration of PVP K30 increased, the lag time increased.52
As the osmotic agent concentration increased, more water imbibes resulting in more osmotic pressure that releases drug through the orifice. The correlation value for zero order was higher for formulation with high osmotic agent.53 The very close R2 values of zero-order and first-order kinetics is attributed to the high solubility of the drug. The drug release was affected by the variation of osmotic pressure. This also confirms the mechanism of release as zero order. The multiple parameters like pH of media, agitation speed showed negligible role on drug release. As the osmotic pressure of the medium increased rivastigmine release decreased significantly. The in vivo results of rivastigmine osmotic tablet showed 1.79 folds increase in AUC0-24 against pure suspension and 1.53 folds increase against marketed formulation confirms enhanced absorption of rivastigmine for 24 hr. For RHT optimized tablet, stability study indicated a negligible alteration in drug content and drug dissolution during six months of their storage under stressed conditions and confirmed the retaining of rivastigmine.
CONCLUSION
The proposed RHT osmotic tablet provided controlled release of rivastigmine over 24 hr independent of pH and agitation intensity. The pre-compression and post-compression parameters were satisfactory. From overlay plot, F2C4 formulation with 20% sodium chloride and 1% PVP K30 was optimized. Once-daily rivastigmine tablet can be used for efficient treatment of Parkinson’s disease reducing patient compliance.
Cite this article:
Naz A, Subrahmanyam CVS, Rachamalla SS. Development and Characterization of Rivastigmine Hydrogen Tartrate Elementary Osmotic Tablets. Int. J. Pharm. Investigation. 2024;14(1):239-49.
ACKNOWLEDGEMENT
The authors thank UCT, Osmania University for extended support during the research work.
ABBREVIATIONS
| EOP | Elementary osmotic tablet |
|---|---|
| RHT | Rivastigmine hydrogen tartrate |
| PVP K30 | Polyvinyl pyrrolidine K30 |
| PEG 400 | Polyethylene glycol 400 |
| ODD | Osmotic drug delivery |
| IAEC | Institutional Animal Ethics Committee |
| FTIR | Fourier transform infrared spectroscopy |
| DSC | Differential scanning calorimetry |
| SEM | Scanning Electron Microscopy |
References
- . Chapter 22. Array. 2003 [Google Scholar]

- Theeuwes F. Elementary osmotic pump. J Pharm Sci. 1975;64(12):1987-91. [PubMed] | [CrossRef] | [Google Scholar]

- Prabakaran D, Singh P, Kanaujia P, Vyas SP. Effect of hydrophilic polymers on the release of diltiazem hydrochloride from elementary osmotic pumps. Int J Pharm. 2003;259(1-2):173-9. [PubMed] | [CrossRef] | [Google Scholar]

- Nguyen K, Hoffman H, Chakkamparambil B, Grossberg GT. Evaluation of rivastigmine in Alzheimer’s disease. Neurodegener Dis Manag. 2021;11(1):35-48. [PubMed] | [CrossRef] | [Google Scholar]

- . Bradley and Daroff’s Neurology in clinical practice. 2022:1452-97. [PubMed] | [CrossRef] | [Google Scholar]

- Simon A, Amaro MI, Healy AM, Cabral LM, de Sousa VP. Comparative evaluation of rivastigmine permeation from a transdermal system in the Franz cell using synthetic membranes and pig ear skin with correlation. Int J Pharm. 2016;512(1):234-41. [PubMed] | [CrossRef] | [Google Scholar]

- Lee L, Hossain M, Wang Y, Sedak g. Absorption of rivastigmine from different regions of GI in humans. J Clin Pharmacol. 2004;44:599-604. [PubMed] | [CrossRef] | [Google Scholar]

- Kapil R, Dhawan S, Singh B, Garg B, Singh B. Systematic formulation development of once-a-day gastroretentive controlled release tablets of rivastigmine using optimized polymer blends. J Drug Deliv Sci Technol. 2012;22(6):511-21. [CrossRef] | [Google Scholar]

- . Naturally occurring chemical against Alzheimers disease. 2021:93-108. [CrossRef] | [Google Scholar]

- Sadowsky CH, Micca JL, Grossberg GT, Velting DM. Rivastigmine from capsules to patch: therapeutic advances in the management of Alzheimer’s disease and Parkinson’s disease dementia. Prim Care Companion CNS Disord. 2014;16(5):25667813 [PubMed] | [CrossRef] | [Google Scholar]

- Emre M, Poewe W, De Deyn PP, Barone P, Kulisevsky J, Pourcher E, et al. Long-term -safety of rivastigmine in Parkinson disease dementia: an open-label, randomized study. Clin Neuropharmacol. 2014;37(1):9-16. [PubMed] | [CrossRef] | [Google Scholar]

- Lefèvre G, Sedek G, Jhee SS, Leibowitz MT, Huang HL, Enz A, et al. Pharmacokinetics and pharmacodynamics of the novel daily rivastigmine transdermal patch compared with twice-daily capsules in Alzheimer’s disease patients. Clin Pharmacol Ther. 2008;83(1):106-14. [PubMed] | [CrossRef] | [Google Scholar]

- Hsieh SW, Chen JC, Chen NC, Jhang KM, Wang W, Yang YH, et al. Real-world evaluation of tolerability, safety and efficacy of rivastigmine oral solution in patients with mild to moderate Alzheimer’s disease dementia. Clin Psychopharmacol Neurosci. 2021;19(3):459-69. [PubMed] | [CrossRef] | [Google Scholar]

- Kapil R, Dhawan S, Beg S, Singh B. Buccoadhesive films for once-a-day administration of rivastigmine: systematic formulation development and pharmacokinetic evaluation. Drug Dev Ind Pharm. 2013;39(3):466-80. [PubMed] | [CrossRef] | [Google Scholar]

- Razack MA, Prasad GS, Raju SSRK. Design, optimization, development and evaluation of once a day controlled release formulation of rivastigmine hydrogen tartrate. J Drug Deliv Ther. 2014;4(6):58-67. [PubMed] | [CrossRef] | [Google Scholar]

- Ogorka J, Kalb O. New controlled release oral formulations for rivastigmine. EP Pat. EP 1121104 B1.1-18. 2005 [PubMed] | [CrossRef] | [Google Scholar]

- Park S. Rivastigmine containing sustained release pharmaceutical composition. EP Pat. EP 3 290 023 B1. 1-11. 2021 [PubMed] | [CrossRef] | [Google Scholar]

- Haider M, Elsayed I, Ahmed IS, Fares AR. In situ-forming microparticles for controlled release of rivastigmine: in vitro optimization and in vivo evaluation. Pharmaceuticals (Basel). 2021;14(1) [PubMed] | [CrossRef] | [Google Scholar]

- Salatin S, Barar J, Barzegar-Jalali M, Adibkia K, Alami-Milani M, Jelvehgari M, et al. Formulation and evaluation of Eudragit RL-100 nanoparticles loaded forming gel for intranasal delivery of rivastigmine. Adv Pharm Bull. 2020;10(1):20-9. [PubMed] | [CrossRef] | [Google Scholar]

- Pagar K, Vavia P. Rivastigmine-loaded L-lactide-depsipeptide polymeric nanoparticles: decisive formulation variable optimization. Sci Pharm. 2013;81(3):865-85. [PubMed] | [CrossRef] | [Google Scholar]

- Fazil M, Md S, Haque S, Kumar M, Baboota S, Sahni JK, et al. Development and evaluation of rivastigmine loaded chitosan nanoparticles for brain targeting. Eur J Pharm Sci. 2012;47(1):6-15. [PubMed] | [CrossRef] | [Google Scholar]

- Ismail MF, Elmeshad AN, Salem NA. Potential therapeutic effect of nanobased formulation of rivastigmine on rat model of Alzheimer’s disease. Int J Nanomedicine. 2013;8:393-406. [PubMed] | [CrossRef] | [Google Scholar]

- Nagpal K, Singh SK, Mishra DN. Optimization of brain targeted chitosan nanoparticles of rivastigmine for improved efficacy and safety. Int J Biol Macromol. 2013;59:72-83. [PubMed] | [CrossRef] | [Google Scholar]

- Wilson B, Samanta MK, Santhi K, Kumar KP, Paramakrishnan N, Suresh B, et al. Poly(n-butylcyanoacrylate) nanoparticles coated with polysorbate 80 for the targeted delivery of rivastigmine into the brain to treat Alzheimer’s disease. Brain Res. 2008;1200:159-68. [PubMed] | [CrossRef] | [Google Scholar]

- Rompicherla SKL, Arumugam K, Bojja SL, Kumar N, Rao CM. Pharmacokinetic and pharmacodynamic evaluation of nasal liposome and nanoparticle based rivastigmine formulations in acute and chronic models of Alzheimer’s disease. Naunyn Schmiedebergs Arch Pharmacol. 2021;394(8):1737-55. [PubMed] | [CrossRef] | [Google Scholar]

- Arumugam K, Subramanian GS, Mallayasamy SR, Averineni RK, Reddy MS, Udupa N, et al. A study of rivastigmine liposomes for delivery into the brain through intranasal route. Acta Pharm. 2008;58(3):287-97. [PubMed] | [CrossRef] | [Google Scholar]

- Mutlu NB, Değim Z, Yilmaz Ş, Eşsiz D, Nacar A. New perspective for the treatment of Alzheimer diseases: liposomal rivastigmine formulations. Drug Dev Ind Pharm. 2011;37(7):775-89. [PubMed] | [CrossRef] | [Google Scholar]

- Yang ZZ, Zhang YQ, Wang ZZ, Wu K, Lou JN, Qi XR, et al. Enhanced brain distribution and pharmacodynamics of rivastigmine by liposomes following intranasal administration. Int J Pharm. 2013;452(1-2):344-54. [PubMed] | [CrossRef] | [Google Scholar]

- Cunha S, Costa CP, Loureiro JA, Alves J, Peixoto AF, Forbes B, et al. Double optimization of rivastigmine-loaded Nanostructured Lipid Carriers (NLC) for nose-to-brain delivery using the quality by design (QbD) approach: formulation variables and instrumental parameters. Pharmaceutics. 2020;12(7) [PubMed] | [CrossRef] | [Google Scholar]

- Simon A, Amaro MI, Cabral LM, Healy AM, de Sousa VP. Development of a novel dry powder inhalation formulation for the delivery of rivastigmine hydrogen tartrate. Int J Pharm. 2016b;501(1-2):124-38. [PubMed] | [CrossRef] | [Google Scholar]

- Malaiya MK, Jain A, Pooja H, Jain A, Jain D. Controlled delivery of rivastigmine using transdermal patch for effective management of Alzheimer’s disease. J Drug Deliv Sci Technol. 2018;45:408-14. [CrossRef] | [Google Scholar]

- Sadeghi M, Ganji F, Taghizadeh SM, Daraei B. Preparation and characterization of rivastigmine transdermal patch based on chitosan microparticles. Iran J Pharm Res. 2016;15(3):283-94. [PubMed] | [Google Scholar]

- Kumar UG, Rao SK, Kumari HM. Formulation and evaluation of controlled microporous osmotic tablets of rivastigmine hydrogen tartrate. World J Pharm Res. 2014;3(2):2493-503. [PubMed] | [Google Scholar]

- European Pharmacopoeia 9.0 [monograph]: Rivastigmine hydrogen tartrate In: EP 9.0: 3503-3504. [PubMed] | [Google Scholar]

- Liu L, Khang G, Rhee JM, Lee HB. Monolithic osmotic tablet system for nifedipine delivery. J Control Release. 2000;67(2-3):309-22. [PubMed] | [CrossRef] | [Google Scholar]

- Modi CD, Patel DJ, Chaudhary AB, Viramgama PH. Amalgamation of QbD and alcohol Induced dose Dumping Studies on diltiazem hydrochloride Modified Release Tablets. Int J Pharm Investig. 2022;12(4):462-9. [CrossRef] | [Google Scholar]

- Sahoo CK, Rao SRM, Sudhakar M. Formulation and evaluation of controlled porosity osmotic pump tablets for zidovudine and lamivudine combination using fructose as osmogen. J Drug Deliv Ther. 2017;7(4):41-50. [CrossRef] | [Google Scholar]

- Arjun N, Narendar D, Sunitha K, Harika K, Nagaraj B. Development, evaluation, and influence of formulation and process variables on performance of oral elementary osmotic device of atenolol. Int J Pharm Investig. 2016;6(4):238-46. [PubMed] | [CrossRef] | [Google Scholar]

- Kumar P, Singh S, Mishra B. Development and biopharmaceutical evaluation of extended release formulation of tramadol hydrochloride based on osmotic technology. Acta Pharm. 2009;59(1):15-30. [PubMed] | [CrossRef] | [Google Scholar]

- Suryadevara V, Lankapalli SR, Vejella UMR, Mupparaju S, Chava SB. Formulation and evaluation of losartan potassium osmotic controlled matrix tablets. Indian J Pharm Educ. 2014;14 [PubMed] | [CrossRef] | [Google Scholar]

- Xu WJ, Li N, Gao CK. Preparation of controlled porosity osmotic pump tablets for salvianolic acid and optimization of the formulation using an artificial neural network method. Acta Pharmacol Sin B. 2011;1(1):64-70. [CrossRef] | [Google Scholar]

- Nokhodchi A, Momin MN, Shokri J, Shahsavari M, Rashidi PA. Factors affecting the release of nifedipine from a swellable elementary osmotic pump. Drug Deliv. 2008;15(1):43-8. [PubMed] | [CrossRef] | [Google Scholar]

- Gundu R, Pekamwar S, Shelke S, Kulkarni D, Shep S. Development, optimization and pharmacokinetic evaluation of biphasic extended-release osmotic drug delivery system of trospium chloride for promising application in treatment of overactive bladder. Futur J Pharm Sci. 2021;7(1):1-20. [CrossRef] | [Google Scholar]

- Khan ZA, Tripathi R, Mishra B. Design and evaluation of enteric coated microporous osmotic pump tablet (ECMOPT) of quetiapine fumarate for the treatment of psychosis. Acta Pol Pharm. 2012;69(6):1125-36. [PubMed] | [Google Scholar]

- Patel A, Dodiya H, Shelate P, Shastri D, Dave D. Design, characterization, and optimization of controlled drug delivery system containing antibiotic drug/s. J Drug Deliv. 2016;2016 [PubMed] | [CrossRef] | [Google Scholar]

- Arjun N, Narendar D, Sunitha K, Harika K, Nagaraj B. Development, evaluation, and influence of formulation and process variables on performance of oral elementary osmotic device of atenolol. Int J Pharm Investig. 2016;6(4):238-46. [PubMed] | [CrossRef] | [Google Scholar]

- Subrahmanyam CVS, Thimmasetty J, Sathesh Babu PR. Advanced physical pharmaceutics. 2021:303-13. [PubMed] | [CrossRef] | [Google Scholar]

- Saleem MT, Shoaib MH, Yousuf RI, Ahmed FR, Ahmed K, Siddiqui F, et al. SeDeM tool-driven full factorial design for osmotic drug delivery of tramadol HCl: formulation development, physicochemical evaluation, and PBPK modeling for predictive pharmacokinetic evaluation using GastroPlus™. Front Pharmacol. 2022;13:974715 [PubMed] | [CrossRef] | [Google Scholar]

- USP. Metoprolol succinate extended-release tablets. In: USP29-NF24. ;31(1):65 [PubMed] | [CrossRef] | [Google Scholar]

- Bharadwaj P, Upaddhyay PK, Agarwal V, Chaurasia D, Chaurasia H, Singh R, et al. Development and characterization of elementary osmotic pump tablets for simultaneous release of metformin and glipizide. Indian Drugs. 2012;49(11):19-29. [CrossRef] | [Google Scholar]

- Li Y, Pan H, Duan H, Chen J, Zhu Z, Fan J, et al. Double-layered osmotic pump controlled release tablets of actarit: and evaluation. Asian J Pharm Sci. 2019;14(3):340-8. [PubMed] | [CrossRef] | [Google Scholar]

- Xie X, Yang Y, Yang Y, Li Z, Zhang H, Chi Q, et al. The development and evaluation of a subcutaneous infusion delivery system based on osmotic pump control and gas drive. Drug Deliv. 2016;23(7):2193-204. [PubMed] | [CrossRef] | [Google Scholar]

- Vooturi R, Gannu R, Tadishetty A, Rao M. Development of controlled release formulation based on osmotic technology for a phenyl propanalamine hydrochloride: , pharmacokinetic and pharmacodynamic characterization. Acta Pharm Sci. 2011;53(1):25-34. [PubMed] | [CrossRef] | [Google Scholar]


