ABSTRACT
Aim and Objectives
This study examined SSRI-related adverse drug reactions (ADRs), medication adherence, commonly prescribed SSRIs, and gender and age distribution in patients with depression at three tertiary care hospitals in Kerala, India.
Materials and Methods
The prospective observational study was conducted in the psychiatry departments of Al Azhar Medical College Hospital in Thodupuzha, Mount Zion Medical College Hospital in Adoor and Christuraj Hospital in Kottarakara. A predefined WHO form was used to evaluate ADRs. A study-specific data collection form was used to record demographics, clinical details, and prescribed drugs following a unified research protocol. In addition, the WHO causality scale, the Naranjo Probability scale, Hartwig’s severity assessment scale, and the Modified Shumock and Thornton Preventability Scale were also used to evaluate ADRs.
Results
Among the 230 patients (female, 56.52%; depression prevalence age 21-40, 57.83%) who took SSRI, 26.87% reported ADRs. Depressive mood disorder was the most prevalent diagnosis, affecting 47% of patients, followed by generalized anxiety disorder (17.3%). Escitalopram (60.43%) was the most prescribed SSRI for depression, followed by fluvoxamine (21.74%). ADRs were predominantly observed in the cardiovascular, neurological, and gastrointestinal systems. Nausea was the most common ADR (25.77%), followed by insomnia (22.68%), lethargy (16.49%), and headache (11.3%).43% of the ADRs were ‘probable causality.’ Among all the ADRs, 54% were preventable. 64% of the ADRs were mild in their severity. Escitalopram, the most prescribed medication, was the primary cause of ADRs, with fatigue being particularly prevalent. Non-adherence to SSRIs was common, especially with escitalopram, often due to missed doses.
Conclusion
This study shows the prevalence of depressive mood disorders in the population examined. SSRIs like escitalopram and fluvoxamine often cause insomnia and nausea when prescribed for depression. Clinical pharmacists are crucial to patient counselling and education. Targeted strategies are needed to reduce antidepressant nonadherence due to multiple factors. Given the dangers of untreated depression, such as suicide, public health requires effective depression management.
INTRODUCTION
Depression is a prevalent mental disorder and a leading cause of functional impairment. By 2020, according to the World Health Organization (WHO), it will be the second leading cause of disability worldwide. Depression is characterized by a sad mood, pessimistic thoughts, decreased interest in day-to-day activities, poor concentration, insomnia or increased sleep, significant weight loss or gain, decreased energy, persistent feelings of guilt and worthlessness, decreased libido, and suicidal thoughts that last at least two weeks.1
Patients with depression can be of any gender, age, or background. Fear of stigmatization associated with mental disorders discourages patients from seeking early medical treatment.2 Anti-depressant medications are frequently used in primary care to treat depression. Anti-depressants may effectively treat depression, but patients’ failure to take them as prescribed remains a major barrier to treatment success in clinical practice.3
Anti-depressants are used primarily to treat depression and occasionally to treat anxiety. Anti-depressants are medication that corrects the chemical imbalance of neurotransmitters in the brain responsible for mood and behaviour changes. They are prescribed for various psychiatric disorders, including mild chronic depression, also known as dysthymia and anxiety disorders. Anti-depressants are becoming increasingly popular because they allow patients with depression or other mental disorders to easily overcome their condition.4
In Psychopharmacotherapy, the five main classes of anti-depressants are Monoamine Oxidase Inhibitors (MAOIs), Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs), Tricyclic Anti-depressants (TCAs), Selective Serotonin Reuptake Inhibitors (SSRIs), and atypical anti-depressants.5 Due to its favourable risk-to-benefit ratio, the National Institute for Health and Care Excellence (NICE) treatment guideline 2015 and other studies recommend generic SSRIs as the drug of choice for adults with depression and generalized anxiety disorder.6 Numerous factors, including the patient’s demographics, illness profile, medication side effects, comorbidities, and cost-effectiveness, are considered when choosing an antidepressant for a specific patient.7
The administered drugs may cause several potentially fatal Adverse Drug Reactions (ADR). Although there have been significant advances in our understanding of depressive disorder over the past decade, there are still several unanswered questions regarding disease diagnosis and effective clinical management. In recent years, various drugs from various classes have flooded the market to improve the management of this common disorder. Consequently, monitoring and evaluating prescribing practices and pharmacovigilance studies are necessary to emphasize the rationality of medical care or prompt a corrective message to the prescriber and regulatory authorities.8
Depression has been identified by the World Health Organization (WHO) as one of nine chronic conditions that must be addressed to improve medication adherence. Adherence is “the extent to which a person’s behaviour regarding taking medication, following a diet, or executing a lifestyle (change) corresponds with recommendations from a healthcare provider”.
Depression has been identified by the World Health Organization (WHO) as one of nine chronic conditions that must be addressed to improve medication adherence. Adherence is “the extent to which a person’s behaviour regarding taking medication, following a diet, or executing a lifestyle (change) corresponds with a healthcare provider’s recommendations.” The failure of patients to adhere to medical recommendations increases the risk of relapse and diminishes their quality of life. Many factors, including patient, medication, health system, and social and cultural factors, are associated with anti-depressant non-adherence.9
Therefore, this study aimed to assess the ADR and medication adherence in patients treated with SSRIs for depression and to evaluate the distribution of patients based on gender, age, and other demographics. Additionally, the study aimed to identify the most commonly used drugs within the SSRIs category, assess the impact of medication side effects, comorbidities, and cost-effectiveness on the choice of anti-depressants, and monitor and evaluate prescribing practices and pharmacovigilance studies to improve clinical management of the depressive disorder. Furthermore, the study intended to explore the various factors associated with anti-depressant non-adherence and its impact on the risk of relapse and quality of life of the patients.
MATERIALS AND METHODS
This prospective observational study was conducted in the Psychiatric Departments at Al Azhar Medical College Hospital in Thodupuzha, Kerala, India, Mount Zion Medical College Hospital in Adoor, Kerala, India and Christuraj Hospital in Kottarakara, Kerala, India. Before beginning, the study obtained the necessary administrative and institutional ethics committee approval (AAMC/IEC/2023-2024/12, 14/2023, IEC/CRH 2020/2023) 230 participants were selected based on specific inclusion and exclusion criteria. They were all informed of the study’s objectives and assured of the confidentiality of their data. The patients or their caregivers gave their informed consent, expressed in plain language. Pertinent information was collected using an authorized data collection template. Using a standardized WHO form, adverse drug reactions were recorded, and medication adherence was evaluated using the Medication Adherence Rating Scale (MARS). The data were then statistically analysed using SPSS version 26 of IBM.
Inclusion and Exclusion Criteria
The inclusion criteria were patients diagnosed with depressive disorder who visited the psychiatry department of the participating hospitals. Participants of all ages and both sexes were included in the study. Included were also pregnant women with a diagnosis of a depressive disorder. In addition, participants had to comprehend the purpose of the study and be willing to disclose health information. Additionally, they were required to sign an informed consent document.
Patients diagnosed with cancer and terminally ill patients were excluded from the study. Those clinically determined to be suicidal risk, to the extent that their inclusion in the study was deemed inappropriate, were also excluded. Participants with a history of serious adverse reactions or allergic reactions to the medications under investigation were excluded. Finally, participants with a history of substance abuse were excluded from the study.
Data analysis
The collected data were entered in Microsoft Excel and results were analysed using SPSS version 26 of IBM.
RESULTS
The study included 230 patients who were administered SSRI. Of these, 56.52% (N=130) were female, and 43.48% (N=100) were male. Females were more susceptible to depression than males.
A notable disparity in the prevalence of depression was reported with respect to gender, as women exhibited rates of 12-month depression that were two to three times greater than those observed in men. Regular hormonal shifts are associated with mood variations and symptoms of depression. Furthermore, a correlation exists between depression and several biological elements, including hereditary traits, personal life conditions and experiences, which contribute to an increased susceptibility to this mental health condition.10
The prevalence of depression was significantly influenced by age, a key demographic feature.
The age range of the participants in the study spanned from 15 to 60 years, as indicated in Table 1. A significant proportion of the patient population fell within the age range of 21 to 40 years, frequently experiencing profound sadness or despair that significantly impacted their ability to carry out everyday activities. It is frequently seen that individuals between the ages of 15 and 20 commonly encounter significant variations in mood; nonetheless, it is imperative to maintain a state of alertness in order to identify potential indicators of depression. In the age range of 41 to 60 years, adults frequently face a multitude of challenges that have the potential to trigger depressive symptoms. These challenges encompass the balancing act of caring for children and elderly parents, financial stressors, experiences of social isolation, concerns related to work and relationships, the onset of menopause, the management of significant health conditions, and the burden of fulfilling numerous obligations without any apparent relief in sight.
| Age group | No. of patients (N=230) | Percentage of patients (%) |
|---|---|---|
| 15-20 | 10 | 4.35% |
| 21-40 | 133 | 57.83% |
| 41-60 | 87 | 37.82% |
| Above 60 | Nil | 0% |
Distribution of patients based on age group.
As shown in Table 2, depressive mood disorder emerged as the most prevalent diagnosis among the numerous disorders (major depression) in our study. Out of the 230 patients, a significant portion (N=107) were categorized under the depression phase. The subsequent diagnoses included generalized anxiety, obsessive-compulsive disorder, panic disorder, specific phobias, and post-traumatic stress disorder. Exposure to traumatic or distressing events, such as physical or sexual abuse, the death of a loved one, or financial difficulties, are key contributors to these disorders. Even if anticipated, major life transitions also played a role. In addition, medical conditions such as cancer, stroke, and chronic pain have been identified as possible triggers.
| Diagnosis | No. of patients (N=23O) | Percentage of patients (%) |
|---|---|---|
| Major depression | 107 | 47% |
| Generalized anxiety disorder | 40 | 17.3% |
| Obsessive-compulsive disorder | 30 | 13.04% |
| Panic disorder | 23 | 1% |
| Phobias | 17 | 0.73% |
| Post-traumatic stress | 13 | 0.56% |
Diagnosis pattern among patients.
Due to their general lack of sedative effects, safety at high doses, and superior tolerability with only minor side effects, SSRIs are extensively prescribed. Table 3 depicts the prescription distribution of SSRIs. In this investigation, the SSRIs escitalopram, fluoxetine, fluvoxamine, and sertraline were evaluated. Escitalopram (60.43%) was the most commonly prescribed SSRI for depressive disorders, followed by fluvoxamine (21.74%). Also prevalent was escitalopram (60.43%), followed by fluoxetine at (13.5%) and sertraline (4.3%). For obsessive-compulsive disorder, the most popular anti-depressants were fluoxetine and escitalopram.
| ADR | Escitalopram (136) | Fluoxetine (30) | Fluvoxamine (54) | Sertraline (10) | Total (230) |
|---|---|---|---|---|---|
| Nausea | 10 | 07 | 07 | 02 | 26 |
| Head ache | 05 | 01 | 04 | – | 10 |
| Dry mouth | 08 | – | – | 02 | 10 |
| Insomnia | 10 | 04 | 05 | 01 | 20 |
| Fatigue | 08 | 05 | 03 | – | 16 |
| Vomiting | – | 01 | 02 | – | 03 |
| Stomach pain | – | – | 04 | – | 04 |
| Diarrhoea | – | 02 | 02 | – | 04 |
| Drowsiness | – | 04 | 01 | 05 | |
| Total | 41 | 20 | 31 | 06 | 98 |
SSRIs associated with Adverse Drug Reactions.
ADRs were predominantly observed in cardiovascular, neurological, and gastrointestinal systems. The distribution of patients based on these ADRs is depicted in Table 3. 98 patients out of 230 who were administered SSRIs experienced ADRs. Nausea was the most common adverse drug reaction after administration, accounting for 25.77%, followed by insomnia at 22.68%, lethargy at 16.49% and headache at 11.3%. As the most commonly prescribed medication, escitalopram was also the primary cause of ADRs. Particularly prevalent among SSRI-treated patients was fatigue. Given that SSRIs do not substantially inhibit alpha-1 adrenergic receptors, orthostatic hypotension is uncommon in patients taking these medications.
Figure 1 presents an assessment of the WHO causality scale of ADR in relation to SSRI. The study utilized the WHO causality scale method to evaluate the ADRs. According to this scale, ADRs can be classified as certain, probable, possible, unlikely, conditional, or assessable. Within this categorization, 32.99% were rated as “possible,” while 24.7% were rated as “probable.” A key distinction between “probable” and “possible” is that the latter might have another equally plausible explanation for the event. Additionally, for “possible,” there might be a lack of information or ambiguity regarding the outcome after discontinuation.
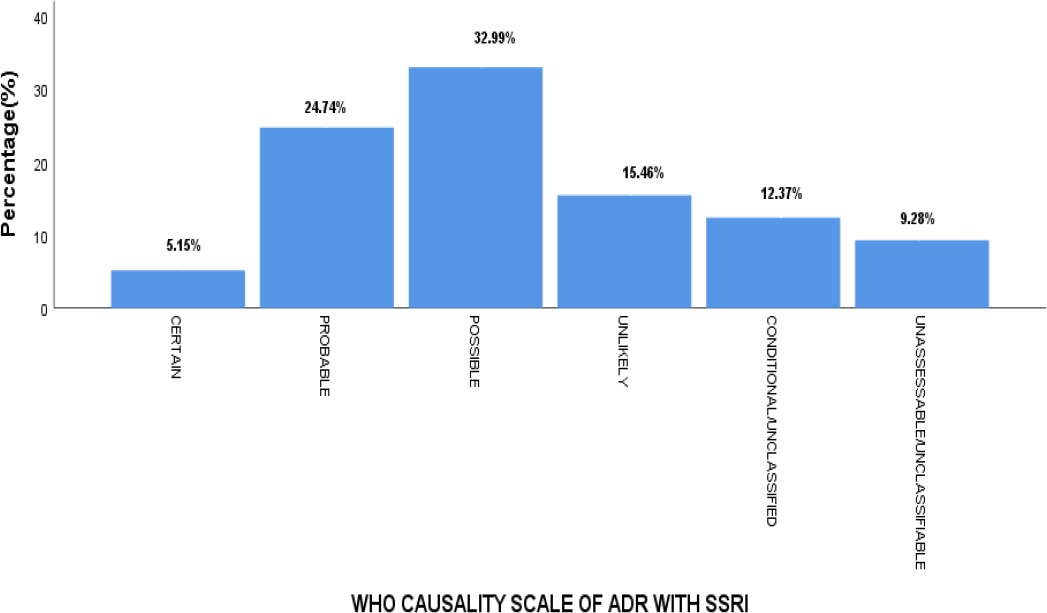
Figure 1.
Assessment of WHO causality scale of ADR with SSRI.
Figure 2 outlines the assessment of ADRs utilizing the Naranjo Probability scale. This scale can classify ADRs as highly probable, probable, or conceivable. In this study, 44.33 percent were categorized as probable, 32.99 percent as conceivable and 22.68 percent as highly probable. The preponderance of ADRs fell into the “probable” classification. The Naranjo ADR Probability Scale was created to standardize the assessment of all adverse drug reactions’ causality. Even though its primary application was intended for controlled trials and the registration of novel medications, it is not typically utilized in routine clinical practice.
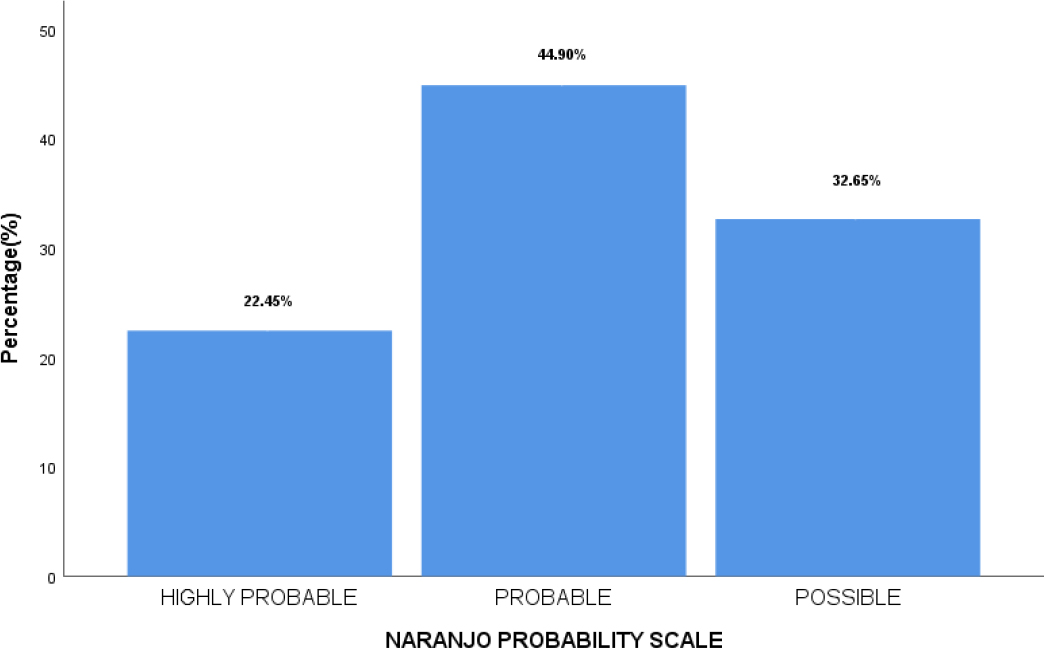
Figure 2.
Assessment of ADR by Naranjo probability scale.
Figure 3 depicts the evaluation of ADR with SSRI using Hartwig’s severity assessment scale, which categorizes adverse reactions as mild, moderate, or severe. In this study, 63.92 percent were classified as moderate, 31.96 percent as mild, and 4.12 percent as severe. Most were categorized as moderate, primarily because the ADR necessitated stopping discontinuing, or modifying the suspected drug treatment.
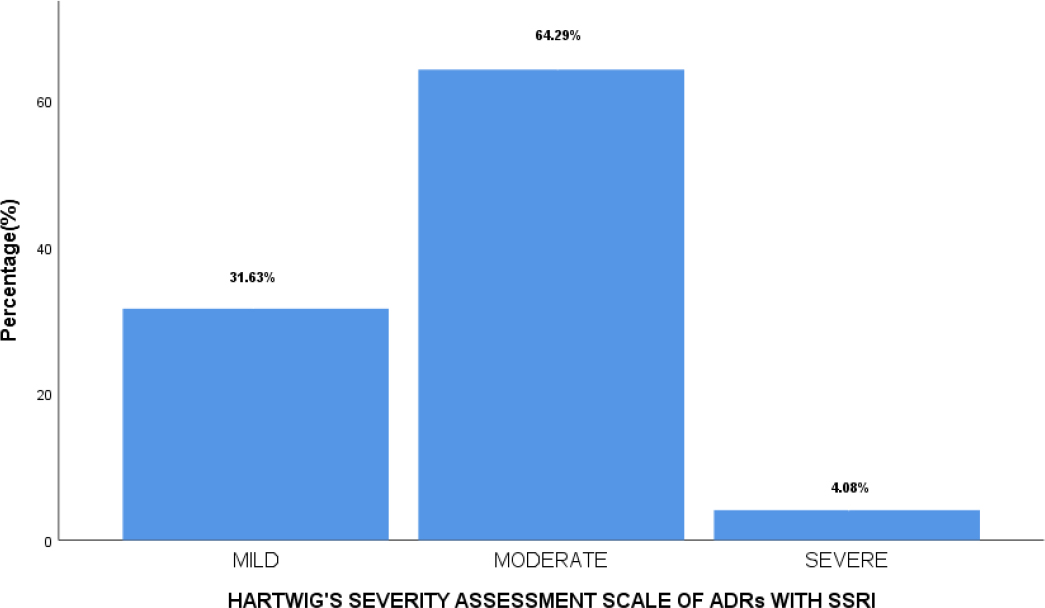
Figure 3.
Assessment of ADR by Hartwig’s Severity assessment scale.
The evaluation of ADR using the Modified Shumock and Thornton Preventability Scale is depicted in Figure 4. While the ADRs were initially evaluated using the WHO scale, the Modified Shumock and Thornton scale categorizes them as either definitely preventable, probably preventable, or not preventable. This analysis determined that 59.79% were possibly preventable, 39.18% were preventable and 1.03% was not preventable. The vast majority of ADRs fell into the “probably preventable” category. These findings provide valuable insights into the nature and characteristics of the ADR, which can influence future clinical decisions and efforts to improve patient safety.
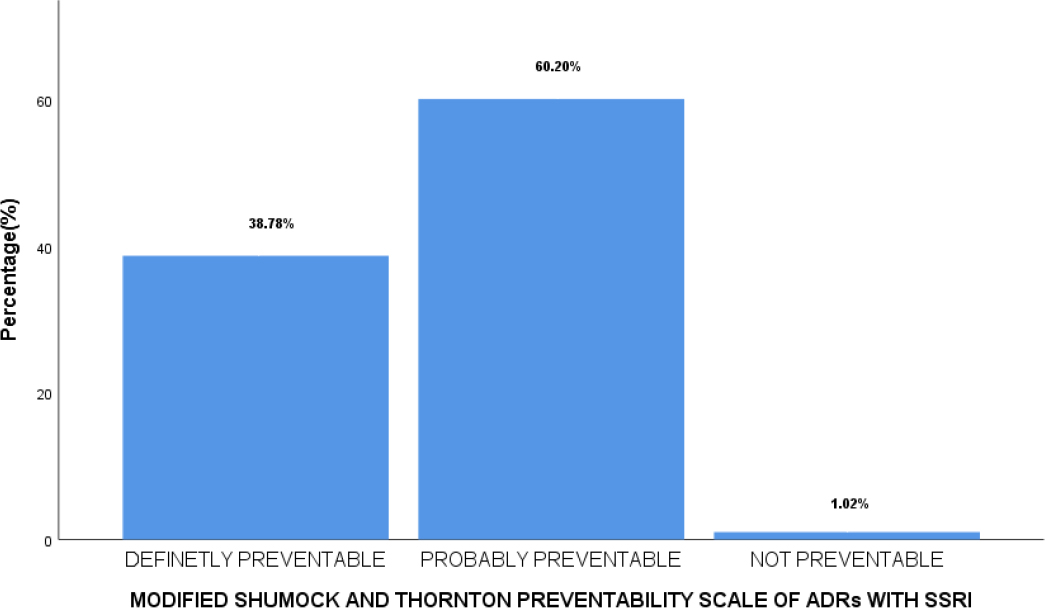
Figure 4.
Assessment of ADR by Modified Shumock and Thornton preventability scale of ADR.
Figure 5a illustrates the levels of nonadherence among patients using SSRIs. The nonadherence was highest with escitalopram, followed by fluvoxamine, often due to behaviours such as missing doses. This study, which examined the effect of anti-depressants on individuals’ work performance, discovered that many were surprised by the medication’s initial adverse effects. These side effects had nearly the same influence on their work capacity as their depressive and anxious symptoms. Nonadherence to anti-depressant treatment is a global problem that prevents patients from receiving optimal care.
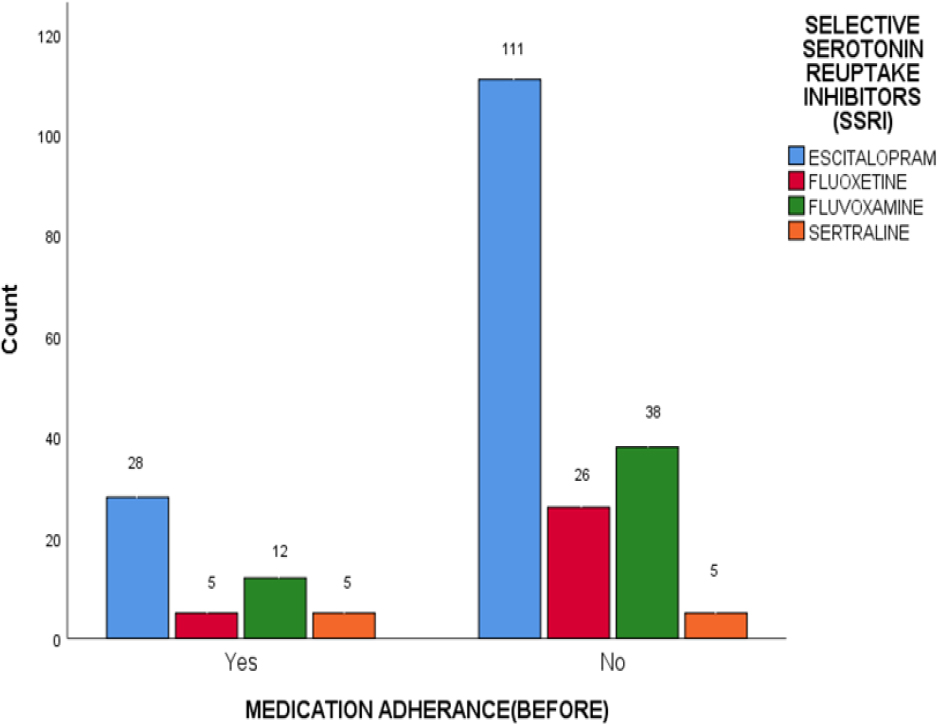
Figure 5 a.
Determination of patients based on Nonadherence with SSRIs.
Figure 5 b shows the levels of medication adherence among patients using SSRIs. Patients receiving escitalopram had a 46% increase in adherence, followed by those receiving fluvoxamine. The Treatment Initiation and Participation Program has effectively increased early pharmacotherapy adherence. Better adherence can enhance depression treatment outcomes. Enhancing medication adherence can impact public health more than individual anti-depressant treatment advancements.
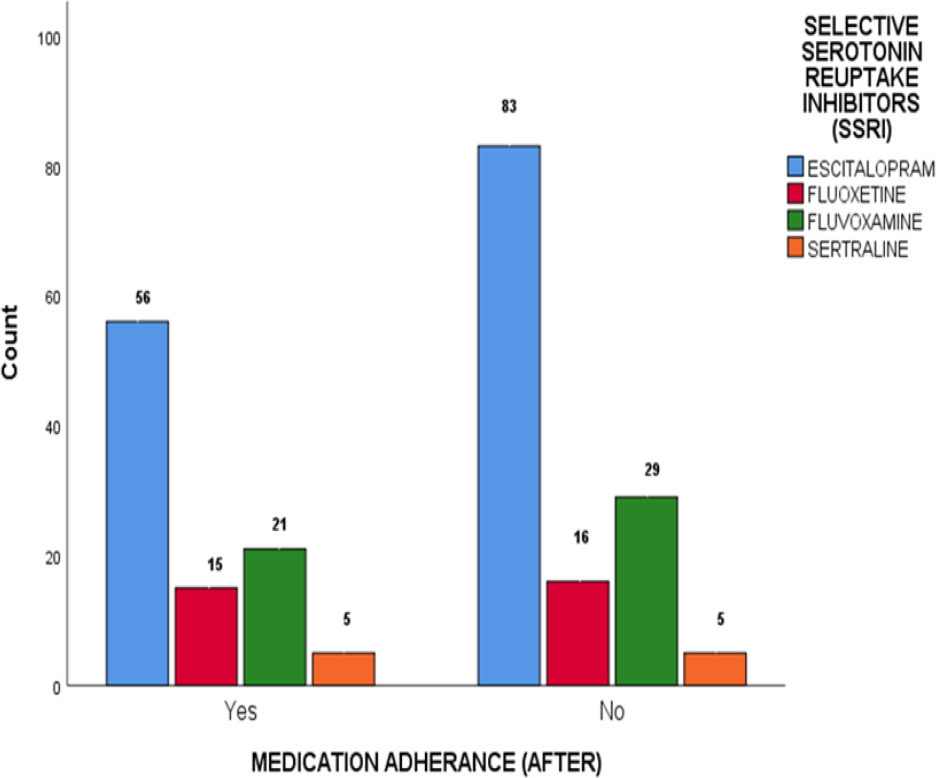
Figure 5 b.
Determination of patients based on Medication Adherence by SSRI.
Figure 5 c depicts the factors that influence nonadherence among SSRI patients. Within patient-related factors, nonadherence was highest for those on escitalopram, followed by fluvoxamine. While many strategies to improve depression outcomes emphasize comprehensive system approaches, such as case identification and intensified monitoring, patients’ willingness to take anti-depressants largely determines the outcome. This preparedness is closely tied to patients’ attitudes toward the medication.
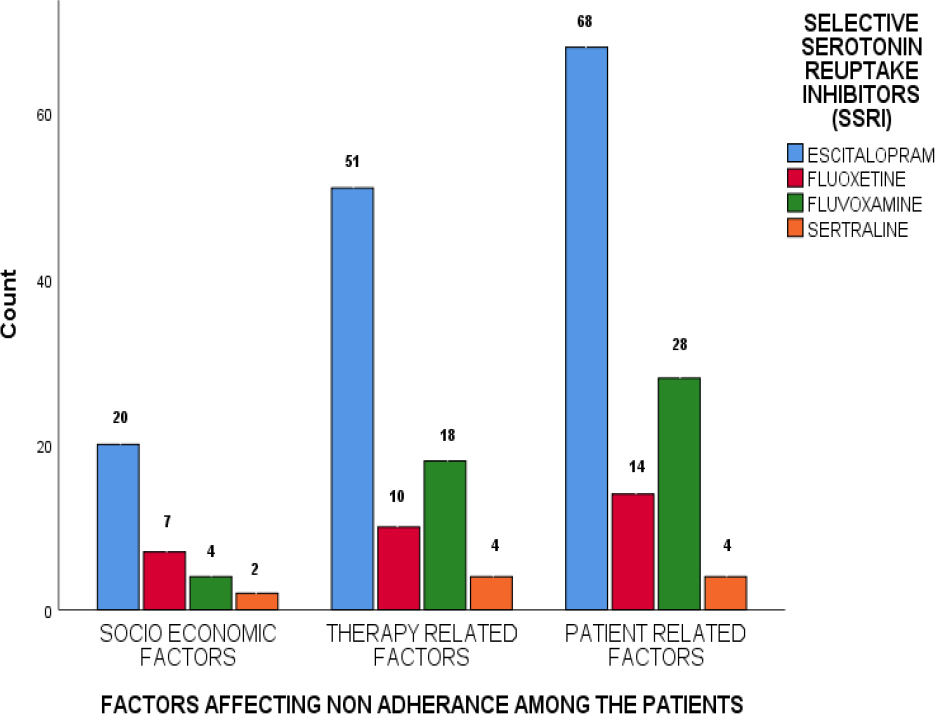
Figure 5 c.
Factors Affecting Nonadherence among the patients with SSRI.
DISCUSSION
Similar research has revealed that sexual dysfunction is a common adverse effect of most conventional anti-depressants, including SSRIs and newer medications. Newer anti-depressants, such as bupropion, may provide effective alternatives with a reduced risk of this side effect. SSRIs rank third in causing ADRs among psychotropic medications, following typical and atypical anti-psychotics. TCAs were associated with a higher incidence of ADR (1.0% of patients) than MAO inhibitors and SSRIs (0.7%; 0.3% for MAO inhibitors and 0.4% for SSRIs.11
It is believed that the differences in depression rates between men and women are related to the hormonal fluctuations associated with the menstrual cycle and pregnancy, which can affect women’s mood. These hormonal changes can cause an imbalance in women’s stress response, making them more prone to depression, especially in stressful situations. Many of the female participants in this study were of childbearing age and had children. However, pregnancy was not a primary cause of depression.12
In our study, the adverse effects of antidepressant use contributed to patient nonadherence. Those prescribed TCA had the highest incidence of adverse effects, followed by those prescribed SNRI and SSRI. Those who were prescribed atypical anti-depressants had the fewest adverse effects. A significant proportion of patients in our study reported weight gain, which led to noncompliance. Negative effects on the central nervous system, such as lethargy and sedation, were major causes of nonadherence. As a result of long-term anti-depressant use, however, many of these patients had developed tolerance to several of these side effects. Only a minority of patients reported having dry mouth. Gastrointestinal issues, such as nausea, abdominal discomfort, and constipation, were common among SSRI users. Patients skipped doses to avoid these side effects. None of the patients with these gastrointestinal disorders adhered to their medication throughout the study. It is essential to inform patients about possible adverse effects so they continue taking their medication despite experiencing these symptoms.
Our research discovered that education level impacted nonadherence most, while other barriers played a lesser role. There’s still an essential position for clinical chemists within the psychiatry department to enhance patient medication adherence. They can accomplish this by raising awareness about the disease and its treatment and providing counselling services to patients.13
Increased awareness may have increased compliance rates. Diverse patient-related and clinician-related factors contribute to either antidepressant adherence or nonadherence. Consequently, both the patient and the prescribing pharmacist/clinician influence adherence. From the patient’s perspective, predominant concerns include apprehensions regarding adverse effects, fears of dependency, and the belief that the medication will not address their particular issues. On the clinician’s side, notable factors include insufficient patient education and inadequate follow-up. As one of the final health professionals’ patients consult, pharmacists have a significant opportunity to improve adherence. They should prioritize ensuring that patients fully comprehend their medication regimens. Pharmacists need to escape from routine, enhance their role in promoting patient adherence, and strengthen their relationship with patients through enhanced monitoring and communication.14
The treatment of depressive disorders remains a challenging task for both patients and physicians. Prior research has demonstrated that a combination of patient education and proactive participation can improve adherence. It is crucial to tailor educational approaches to the patient’s preferences and current stage of change. This study highlights that the preferred educational approach may vary across population.15 The role of a caregiver assuring treatment adherence may vary depending on the severity of depressive symptoms and the degree of functional disability.16
CONCLUSION
Assessing drug utilization provides a deeper understanding of evolving prescription patterns. This study demonstrates that depressive mood disorders are the most prevalent psychiatric diagnosis among the population evaluated. Among anti-depressants, SSRIs, specifically escitalopram and then fluvoxamine, stand out as the most frequently prescribed medications for the treatment of depression. Insomnia and nausea are frequent adverse effects of SSRIs. Clinical pharmacists play a crucial role in raising awareness about the disease and its treatment and providing essential patient counselling services. In addition, this study sheds light on the multitude of factors contributing to antidepressant therapy nonadherence. To improve medication adherence among patients with depression, developing strategies that directly address these factors is vital. Given the potential grave societal consequences of untreated depression, such as suicide, its effective management should be a pillar of national health policies.
Cite this article:
Saji ST, Prasanth VV. Assessment of Medication Adherence and Adverse Drug Reactions in Depressive Patients Taking Selective Serotonin Reuptake Inhibitors in Tertiary Care Hospitals in Kerala. Int. J. Pharm. Investigation. 2024;14(1):232-8.
ACKNOWLEDGEMENT
The authors thank SciWrite Global (www.sciwriteglobal.com), a medical communications company, for the editorial support.
ABBREVIATIONS
| SSRI | Selective serotonin reuptake inhibitors |
|---|---|
| ADR | Adverse drug reaction |
| WHO | World health organisation |
| MAOI | Monoamine oxidase inhibitors |
| SNRI | Serotonin and norepinephrine reuptake inhibitors |
| TCA | Tricyclic anti-depressants |
| NICE | National Institute for Health and Care Excellence |
References
- Mehdi S, Manohar K, Atiqulla S, Shahid Ud, Almuqbil M. Analysis of anti-depressants utilization for patients visiting psychiatric out-patient clinic in a tertiary care hospital healthcare. Int J Med Sci. 2022;10(18):2-13. [Google Scholar]

- Raj N, Sankhi S, Lamichhane R, Marasini Nabin R, Dangi NB, Dangi B, et al. Factors associated with antidepressant medication nonadherence. BioMed Res Int. 2021;8(1):1-8. [Google Scholar]

- Chong WW, Aslani P, Chen TF. Effectiveness of interventions to improve antidepressant medication adherence: a systematic review. Int J Clin Pract. 2011;65(9):954-75. [PubMed] | [CrossRef] | [Google Scholar]

- Aswal N, Singh SK, Kamarapu P. Study on antidepressant drug to cure depression. J Formul Sci Bioavailab. 2018;02(2):1-5. [CrossRef] | [Google Scholar]

- Ali AM, Hendawy AO. So, antidepressant drugs have serious adverse effects, but what are the alternatives. Appro Drug Dev. 2014;4((3)(v)):1-13. [CrossRef] | [Google Scholar]

- Mishra S, Swain TR, Mohanty M. Adverse drug reaction monitoring of anti-depressants in the psychiatry outpatient’s department of a tertiary care teaching hospital. J Clin Diagn Res. 2013;7(6):1131-4. [PubMed] | [CrossRef] | [Google Scholar]

- Tripathi A, Avasthi A, Desousa A, Bhagabati D, Shah N, Kallivayalil RA, et al. Prescription pattern of anti-depressants in five tertiary care psychiatric centres of India. Indian J Med Res. 2016;143(4):507-13. [PubMed] | [CrossRef] | [Google Scholar]

- Kehinde OA, Anyika EN, Abah I. Drug utilization patterns of anti-depressants in Federal Neuro-Psychiatric Hospital Lagos. Niger J Hosp Admin. 2017;6(5):13-9. [PubMed] | [CrossRef] | [Google Scholar]

- Alekhya P, Sriharsha Venkata Ramudu SB, Darsini P. Adherence to antidepressant therapy: sociodemographic factor wise distribution. Int J Pharm Clin Res. 2015;7(3):180-4. [PubMed] | [CrossRef] | [Google Scholar]

- Shrestha Manandhar J, Shrestha R, Basnet N, Silwal P, Shrestha H, Risal A, et al. Study of adherence pattern of anti-depressants in patients with depression. Kathmandu Univ Med J (KUMJ). 2017;15(57):3-9. [PubMed] | [Google Scholar]

- Bohra N, Srivastava S, Bhatia MS. Depression in women in Indian context. Indian J Psychiatry. 2015;57(2) [PubMed] | [CrossRef] | [Google Scholar]

- Tamburrino MB, Nagel RW, Chahal MK, Lynch DJ. Antidepressant medication adherence: A study of primary care patients. Prim Care Companion J Clin Psychiatry. 2009;11(5):205-11. [PubMed] | [CrossRef] | [Google Scholar]

- Marasine NR, Sankhi S. Factors associated with antidepressant medication non-adherence. Turk J Pharm Sci. 2021;18(2):242-9. [PubMed] | [CrossRef] | [Google Scholar]

- Turcu-Stiolicaa A, Adriana-ElenaTaerelb R. Turcu-Stiolica 2014 Identifying and measuring compliance and adherence in anti-depressants taking patients. Procedia Econ Fin. ;15(1):836-9. [PubMed] | [CrossRef] | [Google Scholar]

- Hoffman L, Enders J, Jiacong L, Segal R, Pippins J, Kimberlin C, et al. Impact of an antidepressant management program on medication adherence. Am J Manag Care. 2003;9(1) [PubMed] | [Google Scholar]

- Iris Sher I, Lata McGinn L, Sirey JA JA, Barnett Meyers B. Effects of Ccaregivers’’Pperceived Sstigma and Ccausal Bbeliefs on Ppatients’ Aadherence to Aantidepressant Ttreatment. Psychiatr Serv. 2005;56(5):564-9. 2005 [PubMed] | [CrossRef] | [Google Scholar]


