ABSTRACT
Background
Tuberculosis (TB), a highly contagious and dangerous disease, impacts millions globally, with India topping the list of affected countries. The study aimed to evaluate the knowledge, attitude, practice, and medication adherence of TB patients.
Materials and Methods
A prospective observational study was conducted in total of 150 tuberculosis patients. The study aimed to understand patients’ knowledge, attitude, and practice towards medication and disease, through a binary questionnaire. Medication adherence was assessed using the Medication Adherence Rating Scale (MARS). Based on a 50% cut-off, the knowledge, attitude, practice and medication adherence scores were separated into good and poor categories. Results were analyzed using SPSS and obtained through Chi-Square test, with a p -value<0.05 considered significant.
Results
In this study, the average patient age was 42.27 with a range of 18 to 80, with the largest group being 61 to 70. The highest KAP level was in the 41-50 age group and the lowest in the 71-80 age group. Education level had a significant impact, with 62% being literate and having higher KAP levels than illiterate patients. A significant association was found between home location and KAP level, with 80% of rural patients having lower KAP levels compared to urban residents. The study found no significant relationship between age and medication adherence, but education and location did play a role, with higher education and urban residency linked to better adherence.
Conclusion
Study revealed that pressing need for increased education and awareness about tuberculosis. The disparity in knowledge, particularly about drug-resistant TB, presents a major obstacle to effective management of the disease. The study found that socio-demographic factors, such as education and location, play a crucial role in treatment adherence, with higher levels of knowledge positively impacting adherence. Addressing disparities in these areas is crucial to reducing the spread of TB and improving health outcomes.
INTRODUCTION
Tuberculosis (TB) is a highly contagious and potentially life-threatening disease that affects millions of people worldwide. India continues to be the country with the highest number of TB cases globally, with a staggering 25% of the world’s burden of the disease. In 2020, 2.7 million cases were reported in India. Despite efforts to control its spread, the incidence rate remains high at 430 new cases per 100,000 populations, and the prevalence rate is significant at 690 cases per 100,000 population, according to the latest data from the World Health Organization (WHO).1
The impact of inadequate Knowledge, Attitude, Practice, And Medication Adherence (KAP-MA) among Tuberculosis (TB) patients is significant for both their health and the control of the TB epidemic. TB is highly contagious and requires consistent and proper treatment. However, when patients lack KAP-MA, they are at risk of missing appointments, stopping medication early, and not adhering to recommended health behaviours, leading to poor health outcomes and increased transmission.2,3
Multidrug-Resistant Tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) are forms of Tuberculosis (TB) that are resistant to multiple antibiotics. MDR-TB is defined as TB that is resistant to at least two of the most effective first-line antibiotics, while XDR-TB is resistant to at least two of the most effective first-line antibiotics, as well as at least two of the most effective second-line antibiotics. These forms of TB are a major public health concern as they are more difficult and expensive to treat, and have higher mortality rates compared to drug-sensitive TB. The emergence of MDR-TB and XDR-TB is largely due to the overuse and misuse of antibiotics, as well as poor infection control practices. To effectively control the spread of MDR-TB and XDR-TB, it is important to implement strategies to prevent the emergence and spread of drug-resistant strains. This includes ensuring proper use of antibiotics, improving infection control practices, and expanding access to effective TB diagnosis and treatment. It is also crucial to invest in research and development of new and improved TB drugs to address the growing problem of drug-resistant TB.4
To effectively address the challenges and further improve TB care and control in India, it is crucial to strengthen the NTCP and provide it with the necessary resources and support. Only through a sustained and collaborative effort can India effectively control the spread of TB and reduce the burden of the disease.5 Hence, we planned to conduct a study to assess knowledge, attitude, and practice and medication adherence among tuberculosis patients in tertiary care hospital
MATERIALS AND METHODS
Study area
The study was undertaken at the Vivekananda General Hospital located in Deshpande Nagar, Hubballi, for duration of six months.
Study design and sample size
A prospective observational study was carried out among Tuberculosis (TB) patients. The sample size was calculated using a statistical formula, n=[Z1–α/2]2-p(1-p)/d2, the sample size was rounded of to 150. The participants were selected through a random selection. Participants diagnosed with TB, aged 18+, and with comorbidity were included. With the aim of obtaining a comprehensive understanding of the patients’ knowledge, attitude, and practice towards medication and disease, a thorough survey was conducted. The study was initiated by obtaining informed consent from the participants, followed by administering a questionnaire comprising of 11 questions on knowledge and 7 questions on attitude and practice. The questions were designed in a binary format, with a score of 1 given for a “yes” response and 0 for a “no” response.
Additionally, the level of medication adherence was assessed using the Medication Adherence Rating Scale. Based on a 50% cut-off, the knowledge, attitude, practice and medication adherence scores were separated into good and poor categories. The collected data was entered into Microsoft Excel and later analyzed using the Statistical Package for the Social Sciences (SPSS). The results were obtained through Chi-Square test, providing valuable insights into the patients’ understanding and approach towards medication. A p-value<0.05 was considered.
RESULTS
The study analyzed 150 subjects, with 57% being male and 43% female. The subjects were divided into seven age groups, with the largest group being 61 to 70 years (18%) followed by 21 to 30 years (17%). Of the participants, 62% were literate and 36% were illiterate. 81% were married and 19% were unmarried. The majority of participants (80%) were rural residents, while 20% were urban residents.
Knowledge towards TB
Out of 150 participants, 55% of had good knowledge of TB (Figure 1), while 45% had poor knowledge. This disparity in knowledge is a cause for concern, as it highlights the need for increased education and awareness about the disease. Total of 37% knew that TB can be transmitted through coughing and sneezing, which is a good indication that the participants understand how the disease spreads. On the other hand, only 29% knew that TB can spread between people who live or work together, indicating a gap in understanding of the different modes of transmission. However, the participants demonstrated a good understanding of the common symptoms of TB. In our study, 74% were aware of the symptoms such as bloody sputum, shortness of breath, weight loss, and a cough lasting 2-3 weeks. This is an encouraging sign, as early detection and treatment of TB can improve outcomes for those affected. The participants also had a strong belief in the impact of lifestyle changes on TB conditions. Total of 97% believed that lifestyle changes can improve TB conditions, indicating that they understand the importance of healthy habits in managing the disease. There is still room for improvement in the knowledge of TB among the participants. Only 2% were aware of multi-drug resistant TB (MDR-TB), and just 5% had heard of Directly Observed Therapy (DOT) therapy, indicating that there is a need for increased education and awareness about the different forms of TB and the treatments available.
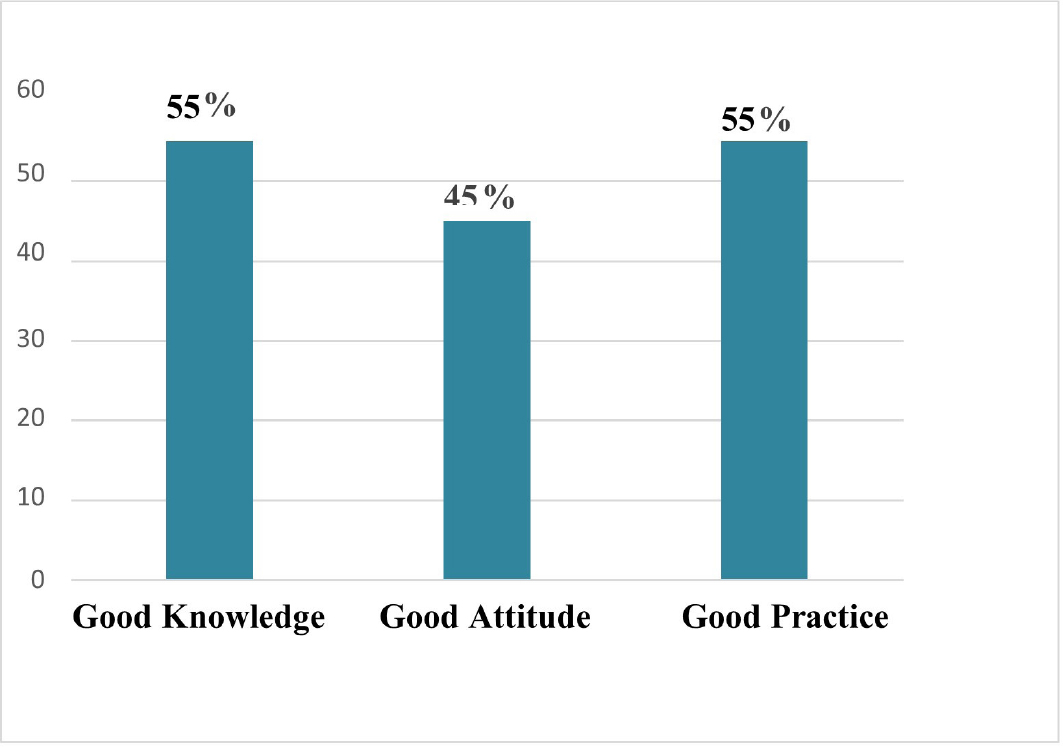
Figure 1:
Overall KAP level for TB.
Attitude towards TB
The study found that a majority of participants considered regular check-ups and completing the full treatment course to be important. This highlights the participants’ understanding of the importance of proper medical care and compliance with treatment regimens. The high percentage of participants who preferred to receive medication and contact a doctor in case of side effects also demonstrates a good understanding of the role of medication in managing TB. However, the study also revealed that a significant portion of the participants thought that isolation from the public would prevent transmission of TB, which is not accurate. This misunderstanding can contribute to the spread of the disease and perpetuate negative attitudes towards those affected. Additionally, the study found that a significant portion of participants considered treatment for TB to be embarrassing, which can discourage individuals from seeking treatment and further contribute to the spread of the disease. However, there is also a significant portion of participants with misconceptions about the disease and negative attitudes towards treatment, which highlights the need for increased education and awareness about TB. Addressing these attitudes is crucial to reducing the spread of the disease and improving outcomes for those affected.
Practice towards TB
The study found that 55% of participants reported good preventive practices towards TB (Figure 1), while 45% reported poor practices. This disparity highlights the need for education and training on effective preventive methods. Of concern, the study found that none of the participants reported participating in a TB awareness program, indicating a lack of access to information and resources on the disease. While 35% of participants agreed to isolate themselves from the public, a high percentage of participants were unaware of the importance of proper isolation as a preventive measure. However, the study also found some positive practices among participants, with 39% reporting that they included multi-grains in their diet and 65% mentioning taking adequate rest and sleep. These healthy habits can contribute to overall health and well-being and can help to prevent the development of TB. The study found that nearly all respondents agreed to follow preventive methods and treatment courses advised by healthcare professionals, indicating a willingness to comply with medical advice and a recognition of the importance of proper treatment.
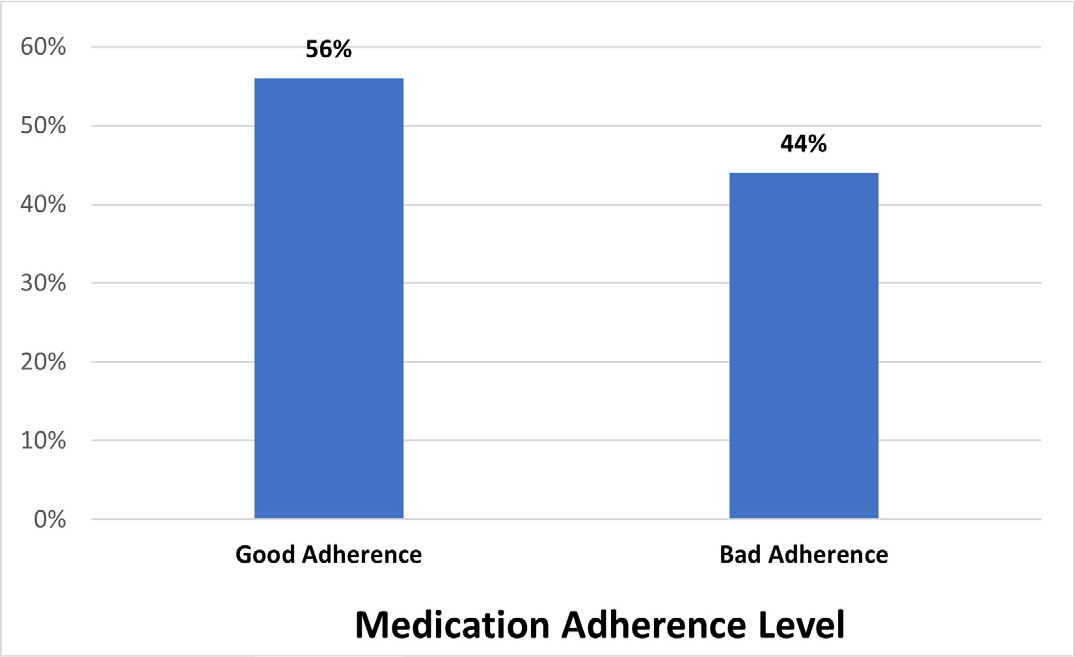
Figure 2:
Overall medication adherence level for TB
Determining the association between KAP and patient socio-demographics
In this study, the average age of patients was found to be 42.27 years old with a range of 18 to 80 years, with the largest group being those aged 61 to 70. The results showed that the highest level of KAP was in the 41-50 age group, while the lowest was in the 71-80 age group.
The study found that education level had a significant impact on the KAP towards TB, with 62% of the participants being literate. The results revealed a lower overall KAP level in illiterate patients compared to literate ones. The study also revealed a significant association between home location and the KAP level towards TB, with 80% of the patients being from rural areas and having lower KAP levels compared to urban residents, who were found to have higher KAP levels for TB (Table 1). The findings of the study indicate that respondents from urban areas had better KAP levels for TB than rural patients, and that education level plays a significant role in determining the level of KAP towards tuberculosis.
Determining the association between medication adherence and patient socio-demographics
The study found no significant relationship between respondent age and TB treatment adherence, but noted that the 31-40 age groups had the highest adherence while the 70-80 age group had the lowest. These findings suggest that age may not be a decisive factor in determining adherence to TB treatment. However, education level was found to have a significant impact on adherence, with higher education leading to improved adherence. Literate participants were also found to display better adherence compared to illiterate ones, highlighting the importance of education in improving treatment outcomes. The study also revealed that location was a factor in adherence, as rural residents were found to have 80% poorer adherence compared to urban residents (Table 1). These findings suggest that urban residency may be linked to better adherence to TB treatment, highlighting the need for targeted interventions and resources in rural areas.
DISCUSSION
The global burden of Tuberculosis (TB) continues to be a major public health concern, with TB being one of the top ten causes of mortality worldwide. The current study aimed to assess the level of knowledge, attitudes, and practices related to TB infection control among study participants.
| Variable | Category | N (%) | Medication Adherence level | Chi-square p value | ||
|---|---|---|---|---|---|---|
| Low | Medium | High | ||||
| Knowledge | Good | 82 (55%) | 5 | 27 | 50 | 0.000* |
| Poor | 68 (45%) | 29 | 23 | 16 | ||
| Attitude | Good | 73 (49%) | 1 | 19 | 53 | 0.000* |
| Poor | 77 (51%) | 33 | 31 | 13 | ||
| Practice | Good | 83 (55%) | 4 | 26 | 53 | 0.000* |
| Poor | 67 (45%) | 30 | 24 | 13 | ||
| Age | <20 | 15 (10%) | 0 | 5 | 10 | 0.001* |
| 21-30 | 26 (17%) | 6 | 8 | 12 | ||
| 31-40 | 21 (14%) | 1 | 5 | 15 | ||
| 41-50 | 23 (15%) | 3 | 8 | 12 | ||
| 51-60 | 23 (15%) | 6 | 9 | 8 | ||
| 61-70 | 27 (18%) | 8 | 11 | 8 | ||
| 71-80 | 15 (10%) | 10 | 4 | 1 | ||
| Gender | Male | 85 (57%) | 20 | 29 | 36 | 0.895 |
| Female | 65 (43%) | 14 | 21 | 30 | ||
| Education | Literate | 96 (64%) | 2 | 37 | 57 | 0.000* |
| Illiterate | 54 (36%) | 32 | 13 | 9 | ||
| Marital status | Married | 121 (81%) | 26 | 42 | 53 | 0.689 |
| Unmarried | 29 (19%) | 8 | 8 | 13 | ||
| Home | Rural | 120 (80%) | 32 | 40 | 48 | 0.040 |
| location | Urban | 30 (20%) | 2 | 10 | 18 |
Association between KAP levels and patient demographics with medication adherence.
It is widely recognized that knowledge is a key factor in shaping people’s attitudes and practices related to infection prevention. The overall knowledge of TB in the current study was 55%, which was lower than what was observed in an Ethiopian study (68%) but higher than in a Thai study (74.2%).6,7 The current study found that 94.6% of participants had heard of TB, which is higher compared to previous studies conducted in other contexts (87.8% in a study in the North Mecha area).8
The findings indicate that the majority of participants in the study had a good understanding of the signs and symptoms of TB, which was similar to what was observed in previous studies conducted in various countries such as Ethiopia, Iran, and the Bhutan.9–11
The overall attitude toward TB in the current study was 49%, which was lower than what was observed in a study conducted in Ethiopia (68%) but higher than in a study conducted in Thailand (47.9%).7,9 The current study found that 55% of participants had good preventive behaviors for TB, which was better compared to a previous study in Iran (42.6%).
The study also found that 7.3% of participants had ever been tested for TB, which was lower compared to a study conducted in Thailand (18.6%).12 Despite having a good understanding of the signs and symptoms of TB, the study revealed knowledge gaps regarding the curability of TB. 14.6% of participants did not know that TB is curable, which is consistent with the findings of a previous study (12%).13
The results of the study raise concern regarding the level of knowledge among participants regarding Drug-Resistant Tuberculosis (MDR-TB). Only 2% of participants were found to be aware of MDR-TB, and a mere 5% had heard of DOT treatment, echoing the findings of a previous study conducted during the Hajj pilgrimage.8 The data indicates a correlation between certain demographic characteristics, such as age, gender, education level, home location, and marital status, and a higher level of awareness regarding TB among participants. This correlation has been supported by similar findings in studies conducted globally.14–17
The persistent issues of re-hospitalization and reinfection of Tuberculosis (TB) caused by non-adherence to treatment remains a major global concern. To assess the extent of treatment adherence among TB patients, the Medication Adherence Rating Scale was used to measure non-adherence. The results of this study revealed a substantial proportion of patients had poor adherence to their TB treatment regimen. The study found that 56% of patients had good adherence and 44 % had bad adherence to the treatment (Figure 2).
These findings contrast with the results of a study in South Africa, which found high levels of adherence to treatment at all follow-up visits during treatment.18 The current study also concluded that there was no significant relationship between age and adherence to TB treatment, consistent with findings from research conducted in Bandung, Indonesia, and Sub-Saharan Africa.19
The current study investigated the relationship between levels of literacy, residency, and knowledge about tuberculosis with adherence to anti-TB medication. The results showed that 64% of the subjects were literate and literate participants were more likely to adhere to their TB treatment regimen than illiterate individuals. This aligns with a similar study conducted in South Africa, which found a strong association between higher levels of education and adherence to TB therapy.20 The study also found that 55% of participants had a strong understanding of tuberculosis, however, those with low levels of knowledge were more likely to have poor adherence. This is consistent with previous studies that have shown a connection between a lack of awareness about tuberculosis and poor adherence to treatment.21,22
CONCLUSION
In conclusion, this study highlights the critical need for education and awareness about tuberculosis and its related issues. The findings show that there is a significant gap in knowledge, attitude, and preventative practices, particularly in rural areas and among the illiterate population. This lack of knowledge, particularly about drug-resistant tuberculosis, poses a significant challenge in effectively managing the disease. The study reveals that socio-demographic factors, including education and location, play a significant role in treatment adherence, with high awareness levels positively associated with better adherence. Addressing disparities in education and location is crucial to improving treatment outcomes and reducing the spread of the disease. The results suggest that there is a strong correlation between knowledge, attitude, and practice levels and medication adherence. Improving these levels is essential to ensure that patients are taking their medications as prescribed, leading to better health outcomes. In light of these findings, continued efforts are needed to address non-adherence through patient education and counselling and to improve the understanding of MDR-TB and its treatment among the general population. Further research is needed to determine effective strategies for improving adherence among high-risk populations.
Cite this article
Nyamagoud SB, Swamy AHV, Chathamvelli A, Patil K, Pai A, Baadkar A. Assessment of Knowledge, Attitude, Practice and Medication Adherence among Tuberculosis Patients in Tertiary Care Hospital. Int. J. Pharm. Investigation. 2024;14(1):135-40.
ACKNOWLEDGEMENT
The authors are thankful to the Vice-Chancellor, Registrar and Dean of Pharmacy, KLE Academy of Higher Education and Research, Belagavi. We would also like to thank Medical and Hospital Staff of Vivekanand General Hospital, Hubballi for providing necessary support.
ABBREVIATIONS
| TB | Tuberculosis |
|---|---|
| KAP | Knowledge, Attitude, and Practice |
| WHO | World Health Organization |
| MDR-TB | Multidrug-resistant tuberculosis |
| XDR-TB | extensively drug-resistant tuberculosis |
| NTCP | National tobacco control programme |
| MMAS-4 | Morisky Adherence Medication Scale (MMAS-4) |
References
- [internet] Who.int. 2021 [cited 2023]. Available from
https://www.who.int/publications-detail-redirect/9789240037021
Global tuberculosis report.
- Dheda K, Gumbo T, Maartens G, Dooley KE, Murray M, Furin J, et al. The Lancet Respiratory Medicine Commission: 2019 update: epidemiology, pathogenesis, transmission, diagnosis, and management of multidrug-resistant and incurable tuberculosis. Lancet Respir Med. 2019;7(9):820-6. [PubMed] | [CrossRef] | [Google Scholar]

- Lu H. Adherence to tuberculosis treatment: A systematic review. Am J Trop Med Hyg. 2018;99(3):767-77. [CrossRef] | [Google Scholar]

- Seung KJ, Keshavjee S, Rich ML. Multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis. Cold Spring Harb Perspect Med. 2015;5(9):a017863 [PubMed] | [CrossRef] | [Google Scholar]

- Gov.in. [cited 2023]. Available from
https://www.nhp.gov.in/revised-national-tuberculosis-control-prog ramme_pg
National tuberculosis elimination programme [internet].
- Kasa AS, Minibel A, Bantie GM. Knowledge, attitude and preventive practice towards tuberculosis among clients visiting public health facilities. BMC Res Notes. 2019;12(1):276 [PubMed] | [CrossRef] | [Google Scholar]

- Sreechat S. Assessment of knowledge, attitude and preventive behavior of pulmonary tuberculosis among Myanmar refugees in Ban Mai Nai Soi temporary shelter, Mae Hong Son, Thailand. J Health Res. 2013;27(6):391-8. [PubMed] | [CrossRef] | [Google Scholar]

- Alotaibi B, Yassin Y, Mushi A, Maashi F, Thomas A, Mohamed G, et al. Tuberculosis knowledge, attitude and practice among healthcare workers during the 2016 Hajj. PLOS ONE. 2019;14(1):e0210913 [PubMed] | [CrossRef] | [Google Scholar]

- Abebe G, Deribew A, Apers L, Woldemichael K, Shiffa J, Tesfaye M, et al. Knowledge, health seeking behavior and perceived stigma towards tuberculosis among tuberculosis suspects in a rural community in southwest Ethiopia. PLOS ONE. 2010;5(10):e13339 [PubMed] | [CrossRef] | [Google Scholar]

- Amiri FB, Doosti-Irani A, Sedaghat A, Fahimfar N, Mostafavi E. Original article knowledge, attitude, and practices regarding HIV and TB among homeless people in Tehran, Iran. Int J Health Policy Manag. 2017;6:1-3. [PubMed] | [CrossRef] | [Google Scholar]

- Dorji T, Tshering T, Wangdi K. Assessment of knowledge, attitude and practice on tuberculosis among teacher trainees of Samtse College of Education, Bhutan. PLOS ONE. 2020;15(11):e0241923 [PubMed] | [CrossRef] | [Google Scholar]

- Pengpid S, Peltzer K, Puckpinyo A, Tiraphat S, Viripiromgool S, Apidechkul T, et al. Knowledge, attitudes, and practices about tuberculosis and choice of communication channels in Thailand. J Infect Dev Ctries. 2016;10(7):694-703. [PubMed] | [CrossRef] | [Google Scholar]

- Yousif TK, Khayat MI, Salman HD. Survey of knowledge, attitude, and practices: enhanced response to TB ACSM, Iraq. Iraq Iraq MEJFM. 2009;7(1):23-38. [PubMed] | [CrossRef] | [Google Scholar]

- Malangu N, Adebanjo OD. Knowledge and practices about multidrug-resistant tuberculosis amongst healthcare workers in Maseru. Afr J Prim Health Care Fam Med. 2015;7(1) [PubMed] | [CrossRef] | [Google Scholar]

- Noé A, Ribeiro RM, Anselmo R, Maixenchs M, Sitole L, Munguambe K, et al. Knowledge, attitudes and practices regarding tuberculosis care among health workers in Southern Mozambique. BMC Pulm Med. 2017;17(1):2 [PubMed] | [CrossRef] | [Google Scholar]

- Hashim DS, Al Kubaisy W, Al Dulayme A. Knowledge, attitudes and practices survey among health care workers and tuberculosis patients in Iraq. East Mediterr Health J. 2003;9(4):718-31. [PubMed] | [CrossRef] | [Google Scholar]

- Hoffman SJ, Guindon GE, Lavis JN, Randhawa H, Becerra-Posada F, Dejman M, et al. Surveying the knowledge and practices of health professionals in China, India, Iran, and Mexico on treating tuberculosis. Am J Trop Med Hyg. 2016;94(5):959-70. [PubMed] | [CrossRef] | [Google Scholar]

- Kastien-Hilka T, Rosenkranz B, Schwenkglenks M, Bennett BM, Sinanovic E. Association between health-related quality of life and medication adherence in pulmonary tuberculosis in South Africa. Front Pharmacol. 2017;8:919 [PubMed] | [CrossRef] | [Google Scholar]

- Du L, Chen X, Zhu X, Zhang Y, Wu R, Xu J, et al. Determinants of medication adherence for pulmonary tuberculosis patients during continuation phase in Dalian, northeast China. Patient Prefer Adherence. 2020;14:1119-28. [PubMed] | [CrossRef] | [Google Scholar]

- Govender S, Mash B. What are the reasons for patients not adhering to their AntiTB treatment in a South African district hospital? South Africa. 2009 [PubMed] | [CrossRef] | [Google Scholar]

- Cherkaoui I, Sabouni R, Ghali I, Kizub D, Billioux AC, Bennani K, et al. Treatment default amongst patients with tuberculosis in urban Morocco: predicting and explaining default and post-default sputum smear and drug susceptibility results. PLOS ONE. 2014;9(4):e93574 [PubMed] | [CrossRef] | [Google Scholar]

- Muture BN, Keraka MN, Kimuu PK, Kabiru EW, Ombeka VO, Oguya F, et al. Factors associated with default from treatment among tuberculosis patients in Nairobi province, Kenya: A case control study. BMC Public Health. 2011;11(1):696 [PubMed] | [CrossRef] | [Google Scholar]


