ABSTRACT
Background
Diabetes is persistent illness that develops mostly when the body produces insufficient amount of the insulin hormone. The insulin hormone regulates blood glucose levels. In recent epidemiological research studies exposed that diabetes patients were likely to experience depression. Independent of glycemic control, insulin therapy, lifestyle variable and diabetes complications, severe hypoglycemia was strongly correlated with the intensity of depressive symptoms in individuals with DM2, who weren’t taking any antidepressants. Aim: The present study aimed to assess the impact of socio-economic status in the elevation of depressive symptoms among diabetes patients.
Materials and Methods
A prospective cross-sectional observational study was conducted for the age of >30 to 100 with sample size of 215.
Results
In our study in age group of 51-70 (52.06%), (72.55%) males, people with positive family history (57.67%), people with co-morbidities (65.49), illiterates (46.51%), skilled workers (37.67%) people with more than 1.80K (40%) showed major depressive symptoms, people with more than 1-5 years durations of disease (55.81%) showed major depression. According to socio-economic scale people belong to (40.93%) upper middle class are more prone to elevated depressive symptoms. According to PHQ-9 scale people showed more mild depression (38.13%).
Conclusion
The study concludes that there are multiple factors like Age, Gender, Family history, Socio-economic status, can leads to depressive symptoms in diabetes patients.
INTRODUCTION
Diabetes is a persistent illness that develops mostly when the body produces insufficient or improper amounts of the hormone insulin or may be ineffective utilization of insulin. During uncontrolled condition that can gravely impair various body systems, including the neurons and blood vessels.1,2
However, diabetic patients are prone to more stress compared with normal people because of maintaining a strict diet and regular exercise to stay in good health, monitoring blood glucose levels, regular follow-up, managing symptoms, and constantly keeping an eye out for complications. As a result, people experience stress, worry, and sadness.3,4
Studies show some evidence that occurrence of depression in diabetes patients is associated with low socio-economic status.
The small evidence base that considers diabetes and depression in low and middle income countries is out of step with the scale of the burden of disease.5,6
Irrespective of the fact that they received a diabetes diagnosis or not, 90686 participants in recent epidemiological research exposed that diabetes patients were more likely to experience depression. The same analysis revealed that those with diabetes who were aware of it had greater rates of anxiety.7 one argument are that anxiety and sadness are brought on by the psychological strain of having a disease. However, sadness was more common in individuals with previously undetected diabetes and brought on by an unhealthy lifestyle, such as sedentary behavior, a poor diet, or a demanding job.
Independent of glycemic control, insulin therapy, lifestyle variables, and diabetes complications, severe hypoglycemia was strongly correlated with the intensity of depressive symptoms in individuals with DM2, who weren’t taking any antidepressants.8 in individuals with DM2; a meta-analysis study was assessing the connection between neuropathy and depression.9,10
MATERIALS AND METHODS
The cross-sectional observational study was conducted for 6 months from September 2022 to march 2023 in Mamatha General Hospital, Khammam. The sample was selected by taking confidence interval of 5% and a confidence level of 95%. The sample size of our study was 215 Patients. Data was collected by using specially designed data collection form. The severity of depression was assessed by using PHQ-9 scale and socio-economic status evaluated using Modified Kuppuswamy SES scale 2022. The protocol was reviewed and approved by Institutional Ethics Committee (IEC) before the commencement of study.
The statistical analysis will be carried out by using Microsoft Office (MS word, MS Excel, and GraphPad Prism software). A student t-Test was used for data analysis based on observations of random set of variables.
RESULTS
Total of 215 patients, 79 subjects are under the age group 30-50, 10 have no depression, 31 have mild severity, 28 have minimal severity, 5 have moderate severity, 3 have moderately severe depression, followed by 2 have severe depression. Of 112 subjects who are under the age group 51-70, 40 have mild severity 31 have minimal severity, 28 have moderate severity, 5 have moderately severe depression and no depression, followed by 3 have severe depression. 24 subjects under the age group of more than 70, 11 have mild severity, 5 have minimal and moderate severity, 2 have moderately severe depression, followed by 1 had severe depression, By performing statistical analysis using student t-test, the impact of age distribution on depression in diabetes patients was found to be significant (p value-0.0277) (Table 1).
| Variables | N | % | Gradation of severity | P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No depression | Minimal | Mild | Moderate | Moderately severe | Severe | ||||
| Age | |||||||||
| 30-50 | 79 | 36.74 | 10 | 28 | 31 | 5 | 3 | 2 | 0.0277 |
| 51-70 | 112 | 52.09 | 5 | 31 | 40 | 28 | 5 | 3 | |
| >70 | 24 | 11.16 | 0 | 5 | 11 | 5 | 2 | 1 | |
| Gender | |||||||||
| Male | 156 | 72.55 | 9 | 46 | 66 | 25 | 7 | 3 | 0.08 |
| Female | 59 | 27.44 | 4 | 19 | 16 | 13 | 3 | 4 | |
Impact of age and gender on depression in diabetic patients.
Among 156 male patients, 66 have mild severity, 46 have minimal severity, 25 have moderate severity, 10 have no severity, 9 have no depression, 7 have moderately severe depression, followed by 3 have severe depression. Of a total of 59 female patients, 19 have minimal severity,16 have mild severity,13 have moderate severity, 4 have severe and no depression, followed by 3 have moderately severe depression, By performing statistical analysis using student t-test, the impact of Gender distribution on depression in diabetes patients was found to be significant (p value-0.08) (Table 1).
Among 124 patients with a family history, 44 have mild severity, 41 have minimal severity, 20 have moderate severity, 9 have no depression, followed by 5 have moderately severe and severe depression. Among 91 patients with no family history, 38 have mild severity, 24 have minimal severity, 18 have moderate severity, 6 have moderately severe depression, 4 have no depression, followed by 1 had severe depression, by performing statistical analysis using student t-test, the impact of family history on depression in diabetes patients was found to be significant (P value-0.042) (Table 2).
| Variables | N | % | Gradation of severity | P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No depression | Minimal | Mild | Moderate | Moderately severe | Severe | ||||
| Family history | |||||||||
| Yes | 124 | 57.67 | 9 | 41 | 44 | 20 | 5 | 5 | 0.042 |
| No | 91 | 42.32 | 4 | 24 | 38 | 18 | 6 | 1 | |
| Co morbidities | |||||||||
| Yes | 127 | 65.49 | 6 | 42 | 43 | 22 | 8 | 6 | 0.032 |
| No | 88 | 34.50 | 8 | 23 | 37 | 16 | 2 | 2 | |
Impact of Family history and co morbidities on depression in diabetic patients.
Among 127 comorbid patients, 43 have mild severity, 42 have minimal severity, 22 have moderate severity, 8 have moderately severe depression, followed by 6 have severe and no depression. Among 88 no-comorbid patients, 37 have mild severity, 23 have minimal severity, 16 have moderate severity, 8 have no depression, followed by two have severe and moderately severe depression. The impact of Co-morbidities on depression in diabetes patients was found to be significant (p value-0.032) (Table 2).
Among 36 lower middle-class patients, 15 have minimal severity, 13 have mild severity, 4 have moderate severity, 2 have moderately severe depression, followed by 1 had severe and no depression severity. Among 11 lower-class patients, 6 have minimal severity, 3 have mild severity, followed by 2 have moderate severity. Among 63 upper-lower-class patients, 18 have mild severity, 16 have minimal severity, 17 have moderate severity, 7 have moderately severe depression, 3 have severe depression, followed by 2 have no depression. Among 88 upper-middle-class patients, 45 have mild severity, 20 have minimal severity, 13 have moderate severity, 8 have no depression, followed by 1 had moderately severe and severe depression severity. Among 17 upper-class patients, 9 have minimal severity, 3 have mild severity, 2 have moderate and no severity, followed by 1 had to severe depression severity, by performing statistical analysis using student t-test, the impact of socio economic status on depression in diabetes patients was found to be significant (p value-0.022) (Table 3).
| Variables | N | % | Gradation of severity | P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No depression | Minimal | Mild | Moderate | Moderately severe | Severe | ||||
| Socio economic status | |||||||||
| Lower middle class | 36 | 16.74 | 1 | 15 | 13 | 4 | 2 | 1 | 0.022 |
| Lower class | 11 | 5.11 | 0 | 6 | 3 | 2 | 0 | 0 | |
| Upper lower class | 63 | 29.30 | 2 | 16 | 18 | 17 | 7 | 3 | |
| Upper middle class | 88 | 40.93 | 8 | 20 | 45 | 13 | 1 | 1 | |
| Upper class | 17 | 7.90 | 2 | 9 | 3 | 2 | 0 | 1 | |
Impact of Socio economic Status on depression in diabetic patients.
Among 100 illiterate patients, 37 have mild severity, 27 have minimal severity, 23 have moderate severity, 6 have moderately severe depression, 4 have no depression, followed by 3 have severe depression. 4 primary schooled patients, 3 have mild severity, and 1 has minimal severity. Of 14 middle schooled patients, 6 have minimal severity, 4 have mild severity, and 2 have moderate and moderately severe depression. Of 41 high schooled patients,18 have mild severity,11 have minimal severity,6 have moderate severity, 4 have no depression, followed by 1 had moderately severe and severe depression. 27 intermediate patients, 11 have mild severity, 8 have minimal severity, 3 have moderate severity, 1 had moderately severe depression, followed by 2 have severe and no depression. Of 25 graduates, 10 have minimal severity, 8 have mild severity, 4 have moderate severity, followed by 3 have no depression. Of 4 postgraduates, 2 have mild and minimal severity, by performing statistical analysis using student t-test, the impact of education on depression in diabetes patients was found to be significant (p value-0.044) (Table 4).
| Variables | N | % | Gradation of severity | P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No depression | Minimal | Mild | Moderate | Moderately severe | Severe | ||||
| Education | |||||||||
| Illiterate | 100 | 46.51 | 4 | 27 | 37 | 23 | 6 | 3 | 0.044 |
| Primary school (1-4) | 4 | 1.86 | 0 | 1 | 3 | 0 | 0 | 0 | |
| Middle school (4-7) | 14 | 6.51 | 0 | 6 | 4 | 2 | 2 | 0 | |
| High school (7-10) | 41 | 19.06 | 4 | 11 | 18 | 6 | 1 | 1 | |
| Intermediate diploma | 27 | 12.55 | 2 | 8 | 11 | 3 | 1 | 2 | |
| Graduate | 25 | 11.62 | 3 | 10 | 8 | 4 | 0 | 0 | |
| Postgraduate | 4 | 1.86 | 0 | 2 | 2 | 0 | 0 | 0 | |
| Occupation | |||||||||
| Unemployed | 1 | 16 | 17 | 8 | 2 | 2 | 1 | 16 | 0.023 |
| Labour | 1 | 3 | 8 | 3 | 1 | 1 | 1 | 3 | |
| Machine Operator | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 1 | |
| Trade workers | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | |
| Farmer | 1 | 8 | 12 | 9 | 5 | 1 | 1 | 8 | |
| Skilled workers | 7 | 28 | 34 | 10 | 2 | 0 | 7 | 28 | |
| Clerks | 0 | 1 | 4 | 0 | 0 | 1 | 0 | 1 | |
| Technicians | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | |
| Professionals | 2 | 7 | 5 | 4 | 0 | 1 | 2 | 7 | |
| Senior officials | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 2 | |
| Income | |||||||||
| ≤9k | 6 | 2.79 | 0 | 4 | 2 | 0 | 0 | 0 | .0182 |
| 9k to 27k | 33 | 15.34 | 0 | 11 | 9 | 10 | 2 | 1 | |
| 27k to 46k | 43 | 20 | 1 | 13 | 12 | 10 | 4 | 3 | |
| 46k to 68k | 33 | 15.34 | 2 | 10 | 15 | 3 | 3 | 0 | |
| 68k to 92k | 4 | 1.86 | 0 | 1 | 1 | 2 | 0 | 0 | |
| 92k to 1.80k | 10 | 4.65 | 1 | 3 | 6 | 0 | 0 | 0 | |
| ?1.80k | 86 | 40 | 9 | 23 | 38 | 13 | 1 | 2 | |
Impact of Education, Occupation and income on depression in diabetic patients.
Among 46 unemployed patients, 17 have mild severity, 16 have minimal severity, 8 have moderate severity, 2 have moderately severe and severe depression, followed by 1 had no depression. Among 17 labourers, 8 had mild severity, 3 have minimal and moderate severity, followed by one had moderately severe, severe, and no depression. Of 3 machine operators, 2 have moderate severity and one had minimal severity. Among 2 trade workers, 1 had moderate severity and 1 had mild severity. Of 36 farmers, 12 have mild severity, 9 have moderate severity, 8 have minimal severity, 5 have moderately severe depression, and 1 had severe and no depression severity. Among 81 skilled workers, 34 have mild severity, 28 have minimal severity, 10 have moderate severity, 7 have no depression severity, followed by 2 have moderately severe depression severity. among 6 clerks, 4 had mild severity, 1 had minimal severity and 1 had severe depression severity. among 2 technicians, 1 had minimal severity, and 1 had moderate severity. Of 19 professionals, 7 have minimal severity, 5 have mild severity, 4 have moderate severity, 2 have no depression, followed by 1 had severe depression. Among 3 senior officials, 2 have minimal severity, followed by 1 had no depression severity, By performing statistical analysis using student t-test, the impact of Occupation on depression in diabetes patients was found to be significant ( p value-0.023) (Table 4).
Among 6 patients’ income below or equal to 9k, 4 have minimal severity and 2 have mild severity. Of 33 patients’ income between 9k-27k, 11 have minimal severity, 10 have moderate severity, 9 have mild severity, 2 have moderately severe depression, followed by 1 had severe depression. Of 43 patients’ income between 27k-46k, 13 have minimal severity, 12 have mild severity, 10 have moderate severity, 4 have moderately severe depression, 3 have severe depression, followed by 1 had no depression. Of 33 patients’ income between 46k-68k, 15 have mild severity, 10 have minimal severity, 3 have moderately and moderately severe depression, followed by 2 have no depression. Of 4 patients’ income between 68k-92k, 2 have moderate severity, 1 had minimal and mild severity. Among 10 patients of income between 92k-1.80k, 6 have mild severity, 3 have minimal severity, followed by 1 had no depression severity. Of 86 patients with income more than or equal to 1.80k, 38 have mild severity, 23 have minimal depression, 13 have moderate severity, 9 have no depression, 2 have severe depression, followed by 1 had moderately severe depression, by performing statistical analysis using student t-test, the impact of income on depression in diabetes patients was found to be significant (p value-0.0182) (Table 4).
Among 215 DM cases, the data is collected through the PHQ-9 scale, 82 (38.13%) subjects were analyzed to have mild depression. 65 (30.23%) were analyzed to have minimal depression, 38 (17.6%) subjects were analyzed to have moderate depression, 11 (5.11%) subjects were analyzed to have moderately severe depression, 6 (2.79%) subjects were analyzed to have severe depression and 13 (6.04) subjects were analyzed to have no depression (Figure 1).
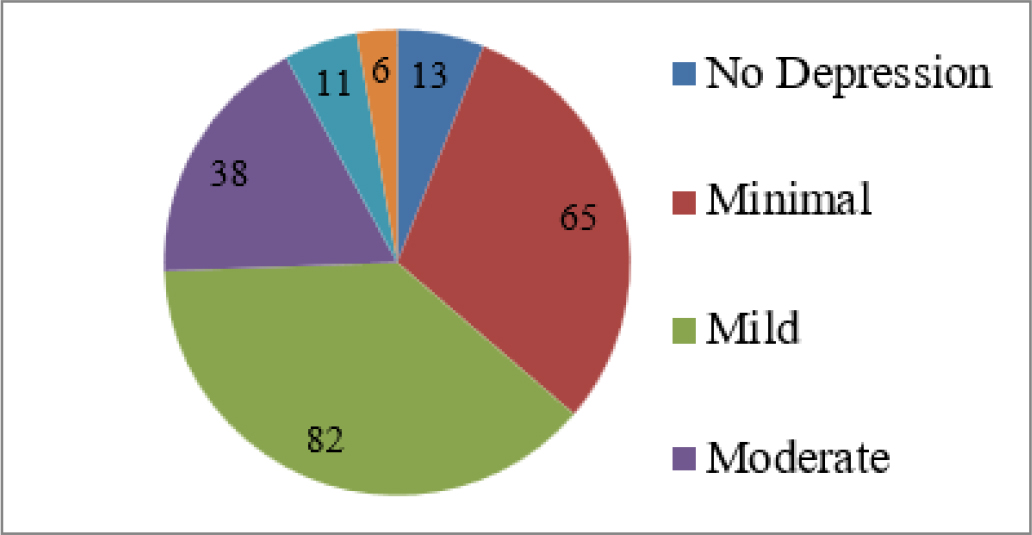
Figure 1.
Severity of depression.
DISCUSSION
The main aim of this research is to determine how frequent depression is among people with diabetes. A standardized questionnaire with several scores depending on parameters including age, gender, co-morbidities, duration of disease, etc. was used to gather the information etc. In this investigation, almost 90% of patients (93.93%) are prone to depression of different grades like minimal (30.23%), mild (38.13%), moderate (17.67%), moderately severe (5.11%), severe (2.79%).
Considering Age as a factor, in the age group of 51-70. Our outcomes presented that age had a significant influence on depression when applied the student T-test for statistical method, with diabetes patients being more likely to be identified with depression (p value=0.027). Opposing this conclusion, abuhegazy H, majairi A, banah F, et al., (2022) concluded that those above the age of 50 had a decreased chance of acquiring depression than those between the ages of 28-40 and In the age group of 51-70.11 because of co-morbidities, loneliness, decreased physical activities, income, education, and other age-related factors have significance in the growth of depression.
Out of 215 DM patients, in our research, we concluded that males have more danger of emerging depression compared with female patients, in the sum of 156 male DM patients 147 developed depression. Gender has significance in the growth of depression when the statistical method was achieved using a student T-test (p value=0.088). Opposing this result deischinger C, dervic E, et al., (2020) concluded that DM is a more solid hazard issue for female depression than male depression.12 In males due to job stress, social standing, income, occupation, and no time to spend with family, with more co-morbidities, have significant progress of depression in DM patients.
In our research, we concluded that people with positive family history (124) of DM have a risk of developing depression, family history has significance in the development of depression when the statistical investigation was accomplished by using the Chi-square ‘P’ test (p value=0.042). Opposing this finding the Nagy G, Rosta K, et al. (2011) asserted that the positive correlation between depression and diabetes mellitus cannot be clarified by hereditary causes.13 Early disease due to family history, and poor medication adherence, has significance in the progress of depression in diabetes patients.
Socio-economic status was determined by considering three factors education, occupation, and income. SES has significance in developing depression when the statistical examination was done by using the student t-test (p value=0.022). Considering these three terms, patients are separated into classes; Patients with lesser revenue have more hazard of emerging depression when compared with people with more income. Similarly, Tiziana leone, Ernestina coast et al. 2012 revealed that depression seemed to be connected with lower SES in diabetes individuals.5 SES doesn’t depend on the country’s economic status, mostly in the case of rural areas people considerably have lower SES compared to urban people with higher SES, in rural areas due to the decreased job opportunities, lower income, illiteracy, and unemployment. In the case of urban areas due to the sedentary lifestyle, and poor physical activities, nowadays due to a lot of screen time, decreased socializing leads to early DM and is connected with depression. People belonging to lower SES and lower-middle-class people have more depression, in the instance of the lower middle class out of 36 patients 35 developed depression of different levels.
It was detected that education has a significant association with the growth of depression (student T-test – p value=0.044). Illiterates have more chance of developing depression because of poor knowledge of the disease and complications of the disease, poor diet plans, little awareness, and poor medication adherence lead to co-morbidities compared with educated people. To prevent this, awareness programs about common diseases should be conducted in rural areas. In the case of hospitals, proper patient counseling about the disease, drug use and adherence in case of disease, should be explained. In the case of educated people, they are aware of the disease and its symptoms. Therefore, early diagnosis is possible and leads to decreased complications due to strict diet and proper medication adherence. Of a full of 100 illiterates, 96 patients have depression of different levels.
The occupation has significance in the growth of depression in diabetes patients when the statistical investigation was completed by student t-test (p value=0.023). Unemployed labourers have more danger of emerging depression when likened with people with stable jobs, unemployed people because economically backward, increased health care cost, significantly affect the patient’s mental status. Labours, because of a lot of physical activities and lesser income and with additional co-morbidities cause depression. In some cases people with stable jobs can also develop depression due to a strict diet and decreased physical activities, with a total of 46 unemployed DM patients 45 have depression of different levels.
In our research, we concluded that income has significance in emerging depression when the statistical investigation was done with the help of a student t-test (p value=0.018). Patients with lesser income have the danger of emerging depression linked with people with more income due to stress and hospital expenses, people with additional revenue can also develop depression in some conditions due to early diagnosis of depression, and proper medication and therapy can decrease the symptoms. Lower- income and middle-income patients have more depression than high-income people.
The patients with one or more co-morbidities (out of 127 patients 123 developed depression) have significance in emerging depression when the statistical investigation was completed by using the Chi-square p-test (p value=0.032). Similarly, Tapash Roy et al. 2012 concluded that the number of co-morbidities and diabetes were both substantially linked with depression.14,15 the co-morbidities like HTN, cardiovascular diseases, asthma, and diabetic complications like diabetic foot ulcer, and retinopathy leads to depression in DM patients, patients with more co-morbidity have severe depression related to people with one co-morbidity or no co-morbidities.
CONCLUSION
People with diabetes mellitus frequently experience depression. Based on what we discovered. As a reason, individuals experiencing co-morbidities like diabetes mellitus must undergo a depression examination. We decided that variables like age factor (51-70), gender (males), comorbidities (1 or more), education (illiterates), occupation (unemployed), income, duration of disease (more than 15 years), SES (lower class) have high risk in affecting patients’ mental status. With this discovery, we can support the need to monitor and develop a treatment for those with the mentioned difficulties.
Cite this article:
Pravalika M, Azeenath A, Firdous T, Yeasmin T, Azharuddin M. Socio-economic Status and Depressive Symptoms in Diabetes Patients: A Cross-Sectional Study. Int. J. Pharm. Investigation. 2024;14(1):225-31.
ACKNOWLEDGEMENT
The authors would like to thank the patients for their participation. We would also like to thank M. Chinna Eswaraiah, Principal of Anurag Pharmacy College, and Kodad for his continuous support and guidance in completing the work.
ABBREVIATIONS
| SES | Socio-economic status |
|---|---|
| IEC | Institutional Ethics Committee |
| PHQ | Patient Health questionnaire |
| HTN | Hypertension |
| QOL | Quality of life |
| DM | Diabetes Mellitus |
References
- Miętkiewska M, Miętkiewska M, Uruska A. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2009;32(Suppl 1) Changes in weight and body composition after initiating insulin therapy and their relationship with metabolic control during the first year of type 1 diabetes in adults. InLipoDiab1 Study. J Med Sci. 2021;e531. doi: 10.20883/medical.e531. [PubMed] | [CrossRef] | [Google Scholar]

- Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12) [PubMed] | [CrossRef] | [Google Scholar]

- Adu MD, Malabu UH, Malau-Aduli AEO, Malau-Aduli BS. Enablers and barriers to effective diabetes self-management: A multi-national investigation. PLOS ONE. 2019;14(6) [PubMed] | [CrossRef] | [Google Scholar]

- Leone T, Coast E, Narayanan S, de Graft Aikins A. Diabetes and depression comorbidity and socio-economic status in low and middle income countries (LMICs): a mapping of the evidence. Global Health. 2012;8:39 [PubMed] | [CrossRef] | [Google Scholar]

- Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social determinants of health and diabetes: A scientific review. Diabetes Care. 2020;44(1):258-79. [PubMed] | [CrossRef] | [Google Scholar]

- Holt RI, de Groot M, Golden SH. Diabetes and depression. Curr Diab Rep. 2014;14(6):491 [PubMed] | [CrossRef] | [Google Scholar]

- Zhou Z, Sun B, Huang S, Zhu C, Bian M. Glycemic variability: adverse clinical outcomes and how to improve it?. Cardiovasc Diabetol. 2020;19(1):102 [PubMed] | [CrossRef] | [Google Scholar]

- Bartoli F, Carrà G, Crocamo C, Carretta D, La Tegola D, Tabacchi T, et al. Association between depression and neuropathy in people with type 2 diabetes: a meta-analysis. Int J Geriatr Psychiatry. 2016;31(8):829-36. [PubMed] | [CrossRef] | [Google Scholar]

- González-Castro TB, Escobar-Chan YM, Fresan A, López-Narváez ML, Tovilla-Zárate CA, Juárez-Rojop IE, et al. Higher risk of depression in individuals with type 2 diabetes and obesity: results of a meta-analysis. J Health Psychol. 2021;26(9):1404-19. [PubMed] | [CrossRef] | [Google Scholar]

- Abuhegazy H, Mujairi A, Banah F, Agdi Y, Elkeshishi H, Kamel A, et al. Depression and associated risk factors among Type 2 diabetic patients: a cross sectional study on a convenience sample from the diabetic center, Khamis Mushait; Saudi Arabia. Neuropsychiatr Dis Treat. 2022;18:1975-84. [PubMed] | [CrossRef] | [Google Scholar]

- Deischinger C, Dervic E, Leutner M, Kosi-Trebotic L, Klimek P, Kautzky A, et al. Diabetes mellitus is associated with a higher risk for major depressive disorder in women than in men. BMJ Open Diabetes Res Care. 2020;8(1) [PubMed] | [CrossRef] | [Google Scholar]

- Nagy G, Rosta K, Szémán B, Sasvári-Székely M, Somogyi A. Clinical aspects of the link between diabetes and depression. Orv Hetil. 2011;152(13):498-504. [PubMed] | [CrossRef] | [Google Scholar]

- Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142 [PubMed] | [CrossRef] | [Google Scholar]

- Katon WJ. The comorbidity of diabetes mellitus and depression. Am J Med. 2008;121(11) [PubMed] | [CrossRef] | [Google Scholar]

- Katon WJ. The comorbidity of diabetes mellitus and depression. Am J Med. 2008;121(11) doi: HYPERLINK “https://doi.org/10.1016/j.amjmed.2008.09.008”, PMID HYPERLINK “https://www.ncbi.nlm.nih.gov/pubmed/18954592”. [PubMed] | [CrossRef] | [Google Scholar]


