ABSTRACT
Background
The use of the evidence-based clinical practice recommendations, offer guide on efficient and prompt therapy of Coronary Artery Disorders (CAD), is inconsistent, especially in developing nations. A wide range of pharmacological classes were needed to treat CAD. In economically developed countries, effective methods for their utilisation, diagnosis, assessment, and management are well-defined; nevertheless, in poor countries, they have not yet been fully embraced. Present study aims to study the various categories of the drugs prescribed to the Myocardial Infarction (MI) patients at a tertiary care hospital.
Materials and Methods
We studied trends in drug prescription patterns among 132 eligible patients diagnosed with MI in the current prospective observational study, which was carried out in a teaching hospital with tertiary care facility.
Results
The results of the study represented, male patients over the age of 40 were more likely to have MI. According to a section of the myocardium affected by an infarction, Anterior Wall Myocardial Infarctions (AWMI) account for 60% of all cases, followed by Inferior Wall Myocardial Infarctions (36%) (IWMI).
Conclusion
The most often recommended medications were hypolipidemics, followed by anticoagulants and antiplatelets.
INTRODUCTION
Coronary Artery Disease (CAD), is the predominant cardiovascular disease with a substantial contribution towards cardiovascular morbidity, mortality includes cardiomyopathies, Acute Myocardial Infarction (AMI), angina pectoris, Congestive Heart Failure (CHF), and myocarditis.1 Myocardial Infarction (MI), the most frequent type of CAD, develops when a coronary artery is completely blocked or almost blocked, leading to a substantial reduction in blood flow and the infarction of a portion of the heart muscle that is carried by that artery.2 Acute myocardial infarctions come in two different forms: ST-segment Elevation Myocardial Infarction (STEMI) and Non-ST-segment Elevation Myocardial Infarction (NSTEMI). Unstable angina is comparable to NSTEMI.3
Around 17.5 million people die from these cardiovascular illnesses each year, making them the largest cause of morbidity and mortality in the world. More than 75% of these deaths take place in Low-and Middle-Income Countries (LMIC). Although the death rate due to cardiovascular complications are dropped in several high-income nations, the trend in LMIC has not been the same.1,4–6 Coronary artery disease is the main cause of mortality worldwide, with rates found in LMIC significantly driving this upward trend from 6.1 million deaths in 1990 to 9.5 million in 2016.7 Between 1990 and 2010, the number of healthy life years-lost due to ischemic heart disease increased by 73% in South Asia, one of the world’s most densely populated regions, compared to the global growth of 30%. South Asia also bears the heaviest burden of cardiovascular illnesses internationally.1–11
Furthermore, compared to those from other countries, South Asians have been observed to have their first MI almost ten years earlier.1,13 And today, four out of every five deaths from ischemic heart disease take place in LMIC, primarily impacting working-age people leads to greater financial challenges for the country.14 By 2025, the World Health Organization (WHO) aims to achieve a 25% relative decrease in non-communicable disease related premature mortality among CVD patients between the ages of 50 and 70. As a result, efforts must be focused on lowering the incidence of CVD in LMIC through two main strategies i.e., first, increasing prevention by addressing risk factors and lowering the case fatality rate for the two main causes of death, MI and stroke, and second, enhancing access to treatment that is based on the best available scientific evidence.15
MI has been the most common cardiovascular emergency seen in the emergency department, becoming the leading cause of death due to CVD in India. Although improvements in healthcare systems and the execution of efficient public health policies have reduced the prevalence of MI in industrialized countries, rates are rising in emerging nations like India. Evidence-based clinical practice guidelines provide guidance on effective and timely management of CAD, utilization of which is not consistent particularly in developing countries.16 Therefore, management of MI should be based on evidence derived from the regional clinical trials data or expert opinion and conclusions drawn based on available evidence. Among the available medications, a few are used to terminate the attack of MI (used as and when required bases) while a few are indicated for long-term management to prevent the frequency of the attack and halt the progression of the disease. The various category of drugs includes Angiotensin-Converting Enzyme inhibitors (ACEi)/ Angiotensin-II Receptor Blockers (ARBs), statins, antianginal agents, anticoagulants, antiplatelet medications, adrenergic P-blockers, calcium channel blockers, diuretics, etc. are listed.
Various guidelines are proposed by various agencies across the globe for the effective management of CVD including The American College of Cardiology (ACC), American Heart Association (AHA), European Society of Cardiology (ESC), Society for Cardiovascular Angiography and Interventions (SCAI) while In India, guidelines are set by Association of Physicians of India (API) and Cardiology Society of India (CSI).17
High-income nations have well-established screening, evaluation, and management procedures for CAD, but India has not fully adopted these strategies.18 Research from all across the world shows that statins, antiplatelet medications, ACEi, and P-blockers are still prescribed insufficiently, and reperfusion treatment for acute MI is still remarkably underutilized.1,20 In the current study, we examined trends in the prescription patterns of medications used in MI patients conducted at A Tertiary Care Hospital in the Rayalaseema Region of Andhra Pradesh, India.
MATERIALS AND METHODS
Study design
A 6-month prospective observational study was conducted at the cardiology department of the tertiary care teaching hospital in collaboration with its Clinical Pharmacy department after approval from the Institutional Review Board (IRB). A total of 143 patients were admitted to the medical ward of the cardiology department and were screened. According to the study criteria only 132 patients were carefully chosen for the study.
Inclusion criteria
Patients with age more than 30 years and of either sex with a confirmed diagnosis of myocardial infarction from the cardiology unit.
Exclusion criteria
Patients with CVD other than MI, special populations like all pregnant women, lactating mothers, and seriously and mentally ill patients; patients with other comorbidities were excluded from the study.
Source of data
Data from each patient was collected from respective patient case files and through patient interviews.
Study procedure
The following data were collected and recorded in the predefined data collection form – patient demographic details (name, gender, age, etc.,) and drug details (drug name, dose, dosage form, route, and frequency of administration). Past medication and medical history were also obtained from patients or caretakers through medication history interview forms. The drugs prescribed to each patient were critically analyzed given their indications and evaluated for their rationality (Figure 1).
Statistical analysis
Descriptive statistics (frequency, percentage, mean, etc.,) were used to present the data with the help of Microsoft Office Excel 2019.
RESULTS
A total of 132 case files of MI patients admitted to the medical ward of the cardiology unit of a tertiary care teaching hospital were analyzed. The findings showed that male patients experienced myocardial infarction more frequently than female patients.
Distribution of patients according to age and gender
Male predominance was seen in our study, where 87 patients (65.9%) were male and 45 patients (34.1%) were female, with a male-to-female ratio of 1.9:1 (Figure 2). According to the age-wise assessment, a high prevalence of MI was found in the 41–70-year age group, with a comparatively high dominance of male patients, and a low rate in the 81–90-year age group (Figure 3).
Distribution of type of MI and associated comorbidities
The most prevalent MI type with more than half of the total cases was Anterior Wall MI (AWMI) followed by Inferior Wall MI (IWMI) and an equal percentage of Posterior Wall MI (PWMI) and Anterior Septum MI (ASMI) with three cases each was seen (Figure 4) from the patients. The reported ASMI and PWMI type MI were one and zero respectively among female patients.
From the past medical history analysis various comorbid conditions were found to be associated with MI, hypertension-the most prevalent comorbidity (35%) followed by Type 2 Diabetes mellitus (31%), and both hypertension and Type 2 Diabetes mellitus together (15.2%). Whereas 11 (8.3%) obesity and 13 (9.8%) thyroid disorders were reported from the patients (Figure 5).
The prescribing pattern in MI
Pharmacologic management of MI involves various categories of drugs namely anticoagulants, antiplatelet agents, lipid-lowering agents and nitrates, and thrombolytic agents as shown in Figure 6. Anticoagulant drugs such as heparin were found in 94% of prescriptions. Lipid-lowering drugs like atorvastatin have been prescribed to 91.6% of patients. Whereas antiplatelet drugs like clopidogrel and nitrate like isosorbide were observed each in 42.9% and nitroglycerine in 42% of prescriptions. Other drugs prescribed to MI patients include the thrombolytic agent streptokinase (41%). Two combination products-clopidogrel along with aspirin as dual therapy were found in 45% and atorvastatin, aspirin, and clopidogrel as triple therapy was found in 17% of the prescriptions. Ticagrelor (2.3%) was the least prescribed drug for MI patients in this study (Figure 6).
DISCUSSION
Prescription pattern monitoring studies are an essential tool for evaluating the prescription, distribution and dispensing of medicines in a specific clinical context to promote the sensible use of medications.21 The goal of the current study was to evaluate the methods used in the cardiology department’s medical ward while prescribing medications to MI patients at a tertiary care teaching hospital. A total of 132 patients were surveyed in 6 months duration to assess drug utilization patterns in a patient on MI therapy. And the prevalence of MI according to various patients and disease factors. Pregnant and lactating women are considered as special population. Further, the endocrinology of human pregnancy involves endocrine and metabolic changes that come about as a result of physiological changes at the mother-fetus border which may influence the cardiovascular function of the mother. Moreover, there will be overlapping symptoms of the normal pregnancy and pregnancy associated MI. It’s crucial to distinguish between changes in symptoms, physical examination, Electrocardiogram (ECG), and biomarkers that occur during normal pregnancies and pregnancy associated MI. Dyspnea is generally observed in late phase of pregnancy but related chest discomfort may be a cardiovascular event. ECG abnormalities are observed in normal pregnancies including smaller Q- waves and T-wave inversions.22 Due to these reasons it’s very challenging to distinguish between the normal pregnancy and pregnancy associated MI so, pregnant women were excluded from the study. The prevalence of MI was found high in male patients (65.9%) than in female patients (34.1%) which is following the similar studies conducted by Indrajit K (2020), Vakade KP (2016), Chrysohoou C (2003), and Weidner G (2000), Jousilahti P (1999).1–27 Patients between the ages of 51 to 60 years made up the largest group, followed by those between 61 and 70 and those between 41 and 50, which was shown to be parallel to past studies executed by Mehra A (2020), Siddaruda MB (2017), Deshmukh S (2017), Chaudhari P (2016). These results demonstrate that older age groups have a higher chance of developing Acute Coronary Syndromes (ACS).1–31 Several risk factors may affect the heart’s basic physiology, accelerating the progression of MI. Diabetes and hypertension were clearly proven to have a negative impact on the prognosis of MI patients as pre the studies performed by Mehra A (2020), Vakade KP (2016), George J (2013), Prabhakaran D (2008), Scott IA (2003).28,32–34 However, obesity and thyroid diseases were inadequately related to MI risk, in accordance with a study by Dona S (2020)32 and in disparity to the study engaged by Naveen A (2017).1,35
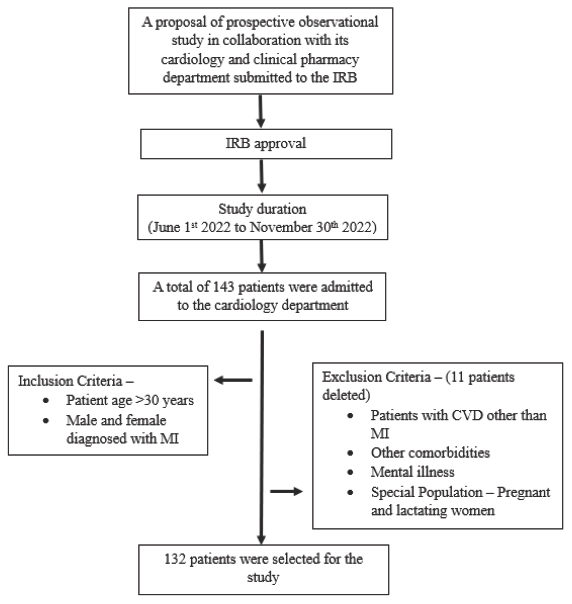
Figure 1:
Study Flow chart
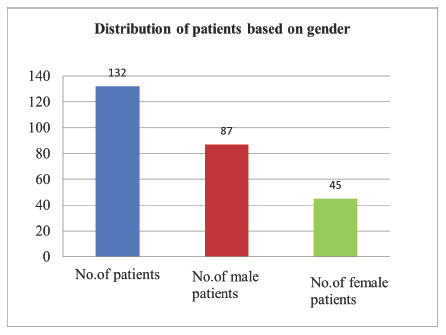
Figure 2:
Distribution of patients based on gender
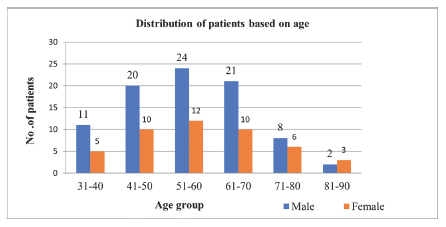
Figure 3:
Distribution of patients based on age group
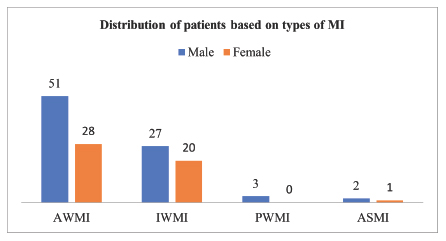
Figure 4:
Distribution of patients based on types of MI
AWMI: Anterior wall myocardial infarctions; IWMI: inferior wall myocardial infarctions; PWMI: percentage of posterior wall MI; anterior septum myocardial infarctions.
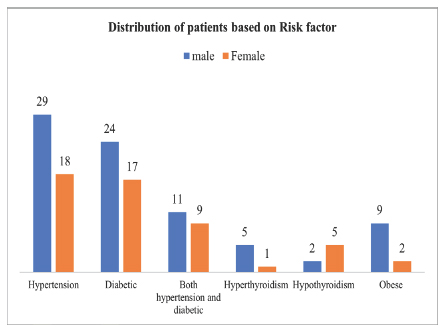
Figure 5:
Distribution of patients based on risk factors
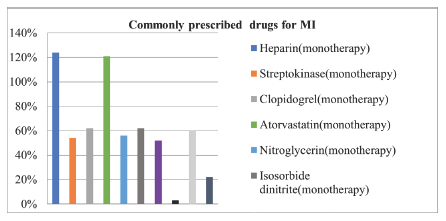
Figure 6:
Commonly prescribed drugs for MI
In the present study incidence of various MI, according to the site all together was anterior wall predominates which was in 62.07% of patients followed by the inferior wall in 35.6%, and a lower incidence was found for the posterior wall (2.27%). These findings were consistent with the study by Ravi Sankar V (2020), Satyanarayan R (2018), Mhatre MA (2016), and Shah MJ (2014).1–39 In our study, the proportion of the prescription of various categories of drugs in MI patients were anticoagulants (94%), and lipid-lowering drugs (91.6%). Whereas antiplatelet drugs (42.9%) and nitrates (42%), thrombolytic agents (41%). Two combination products – clopidogrel along with aspirin as dual therapy were found in 45% and atorvastatin, aspirin, and clopidogrel as triple therapy was found in 17% of the prescriptions. Ticagrelor (2.3%) was the least prescribed drug for MI patients in this study. As per the recommends by Association of Physicians of India (API) all patients with MI should receive dual-antiplatelet¬therapy (DAPT).40 In the present study nearly half of the patients were prescribed DAPT, which was less compared to a study by Dona S (2020)34 and 43% of patients were prescribed Single Antiplatelet Therapy (SAPT) which was very high compared with the same study.
According to a meta-analysis by the Antithrombotic Trialists Collaboration, antiplatelet medication had a considerable positive impact on ACS patients’ outcomes. In the current study aspirin was prescribed to 39% of the patients, aspirin + clopidogrel was prescribed to 45%, clopidogrel was prescribed to 42%, and only ticagrelor was prescribed to three patients (2.27%). In a study by Dona S (2020) and Sandozi T (2010), aspirin monotherapy was prescribed 25.7% of the time and aspirin + clopidogrel together were prescribed to 60% of the MI patients which is comparable to our findings.1–41 Treatment with statins reduces the risk of recurrent MI, CAD, and stroke in previously stabilized ACS patients. High-dose atorvastatin (80 mg) of the statins (among all statins) has been proven to lessen fatalities and ischemia events. The high utilization rate of statins in our study (91.6%) is consistent with the usual recommendations for using the medication in cardiovascular events. The findings were found to be consistent with those of Scott IA (2003) and Dona S (2020).1,35
Nitrates have a long history of utilization in the treatment of cardiovascular disease. Dilating both healthy and stenosed coronary arteries and enhancing coronary collateral flow, continue to play a significant role in modern therapeutic practice. In the current study, nitroglycerin (42%), and isosorbide dinitrate (42.9%) were the two most often prescribed medications. Similar findings were reported by Muhit MA (2012) and Khalid LZ (2013).1,42
CONCLUSION
This study provides insight into drug prescribing patterns and associated comorbidities in MI patients. MI was predominantly seen in male patients, above 40 years of age groups. Based on the segment of the myocardium involved in infarction AWMI accounts for 60% followed by 36% of IWMI. Most prescribed drugs were anticoagulants, and antiplatelets followed by lipid-lowering drugs.
Cite this article
Palli K, Chidrawar V, Veerendra U, Chenchu S, Devangam M, Shiromwar S. Drug Prescribing Pattern in Myocardial Infarction Patients at A Tertiary Care Hospital in South India. Int. J. Pharm. Investigation. 2023;13(4):883-8.
ACKNOWLEDGEMENT
The authors would like to thank the hospital staff and pharmacists working at the hospital, for timely information and cooperation.
ABBREVIATIONS
| ACEi: | Angiotensin-Converting Enzyme inhibitors |
|---|---|
| API: | Association of Physicians of India |
| ARBs: | Angiotensin-II Receptor Blockers |
| AWMI: | Anterior Wall Myocardial Infarctions |
| CAD: | Coronary Artery Disorders |
| CHF: | Congestive Heart Failure |
| CVD: | Cardiovascular Diseases |
| DAPT: | Dual-antiplatelet-therapy |
| IRB: | Institutional Review Board |
| IWMI: | Inferior Wall Myocardial Infarctions |
| LMIC: | Low-and Middle-Income Countries |
| MI: | Myocardial Infarction |
| NSTEMI: | Non-ST-segment Elevation Myocardial Infarction |
| PWMI: | Posterior wall Myocardial Infarctions |
| SAPT: | Single Antiplatelet Therapy |
| CSI: | Cardiology society of India |
References
- World health organization. Global status report on noncommunicable diseases 2014. 2014

- Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O’Neill WW, et al. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000;2000(13):915-22. [PubMed] | [CrossRef] | [Google Scholar]

- Mechanic OJ, Gavin M, Grossman SA. Acute myocardial infarction. 2017 [PubMed] | [CrossRef] | [Google Scholar]

- Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015;2015(17):1667-78. [PubMed] | [CrossRef] | [Google Scholar]

- Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;2015(14):1333-41. [PubMed] | [CrossRef] | [Google Scholar]

- O’Flaherty M, Buchan I, Capewell S. Contributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960s?. Heart. 2013;2013(3):159-62. [PubMed] | [CrossRef] | [Google Scholar]

- Nascimento BR, Brant LCC, Marino BCA, Passaglia LG, Ribeiro ALP. Implementing myocardial infarction systems of care in low/middle-income countries. Heart. 2019;2019(1):20-6. [PubMed] | [CrossRef] | [Google Scholar]

- Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;1998(6):596-601. [PubMed] | [CrossRef] | [Google Scholar]

- Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;27(22):2746-53. [PubMed] | [CrossRef] | [Google Scholar]

- Reddy KS. Cardiovascular disease in non-Western countries. N Engl J Med. 2004;2004(24):2438-40. [PubMed] | [CrossRef] | [Google Scholar]

- Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;2007(3):286-94. [PubMed] | [CrossRef] | [Google Scholar]

- Rehman H, Samad Z, Mishra SR, Merchant AT, Narula JP, Mishra S, et al. Epidemiologic studies targeting primary cardiovascular disease prevention in South Asia. Indian Heart J. 2018;2018(5):721-30. [PubMed] | [CrossRef] | [Google Scholar]

- Ribeiro ALP, Duncan BB, Brant LCC, Lotufo PA, Mill JG, Barreto SM, et al. Cardiovascular health in Brazil: trends and perspectives. Circulation. 2016;2016(4):422-33. [PubMed] | [CrossRef] | [Google Scholar]

- World health organization. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. 2013 [PubMed] | [CrossRef] | [Google Scholar]

- Ajay VS, Prabhakaran D. Coronary heart disease in Indians: implications of the INTERHEART study. Indian J Med Res. 2010;2010(5):561-6. [PubMed] | [CrossRef] | [Google Scholar]

- Jia S, Liu Y, Yuan J. Evidence in guidelines for treatment of coronary artery disease. Adv Exp Med Biol. 2020;1177:37-73. [PubMed] | [CrossRef] | [Google Scholar]

- Association of Physicians of India. API expert consensus document on management of ischemic heart disease. J Assoc Physicians India. 2006;54:469-80. [PubMed] | [Google Scholar]

- Schiele F, Meneveau N, Seronde MF, Caulfield F, Fouche R, Lassabe G, et al. Compliance with guidelines and 1-year mortality in patients with acute myocardial infarction: a prospective study. Eur Heart J. 2005;2005(9):873-80. [PubMed] | [CrossRef] | [Google Scholar]

- Gislason GH, Rasmussen JN, Abildstrøm SZ, Gadsbøll N, Buch P, Friberg J, et al. Long-term compliance with beta-blockers, angiotensin-converting enzyme inhibitors, and statins after acute myocardial infarction. Eur Heart J. 2006;2006(10):1153-8. [PubMed] | [CrossRef] | [Google Scholar]

- Jain S, Upadhyaya P, Goyal J, Kumar A, Jain P, Seth V, et al. A systematic review of prescription pattern monitoring studies and their effectiveness in promoting rational use of medicines. Perspect Clin Res. 2015;2015(2):86-90. [PubMed] | [CrossRef] | [Google Scholar]

- Kumar I, Trishla D, Kumar K. To determine the prescription pattern of drugs used in myocardial infarction in Bihar region: an observational study. Eur J Mol Clin Med (EJMCM). 2020;7(10) [PubMed] | [CrossRef] | [Google Scholar]

- Tweet MS, Lewey J, Smilowitz NR, Rose CH, Best PJM. Pregnancy-associated myocardial infarction: prevalence, causes, and interventional management. Circ Cardiovasc Interv. 2020;13(11) [PubMed] | [CrossRef] | [Google Scholar]

- Mehra A, Bhat NK, Sharma SK, Khajuria K. Drug prescribing pattern in patients of myocardial infarction in a tertiary care teaching hospital of North India. Int J Basic Clin Pharmacol. 2020;2020(9):1357 [CrossRef] | [Google Scholar]

- Vakade KP, Thorat VM, Khanwelkar CC, Jadhav SA, Sanghishetti VM, Veeramachaneni R, et al. A study of prescribing pattern of drugs in patients of cardiovascular emergencies at a tertiary care hospital of Western Maharashtra. Int J Res Med Sci. 2016;2016(2):556-61. [CrossRef] | [Google Scholar]

- Chrysohoou C, Panagiotakos DB, Pitsavos C, Kokkinos P, Marinakis N, Stefanadis C, et al. Gender differences on the risk evaluation of acute coronary syndromes: the CARDIO2000 study. Prev Cardiol. 2003;2003(2):71-7. [PubMed] | [CrossRef] | [Google Scholar]

- Weidner G. Why do men get more heart disease than women? An international perspective. J Am Coll Health. 2000;2000(6):291-4. [PubMed] | [CrossRef] | [Google Scholar]

- Jousilahti P, Vartiainen E, Tuomilehto J, Puska P. Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation. 1999;1999(9):1165-72. [PubMed] | [CrossRef] | [Google Scholar]

- Biradar SM, Pournamy NN, Nayakawadi N, Indu P, Ghodkari MR, Warad V, et al. Prescribing Pattern, Drug Utilization and Clinical Pharmacy Services in Acute Coronary Syndrome patients. Am J Drug Discov Dev. 2017;2017(2):63-9. [CrossRef] | [Google Scholar]

- Deshmukh DS, Deshpande A, Kulkarni ND. Clinical profile of acute myocardial infarction patients from Rural India. J Med Sci Clin Res. 2017;2017(11):30106-11. [CrossRef] | [Google Scholar]

- Choudhary P, Agrawal JM, Malhotra SD, Patel VJ. Drug utilization pattern in acute coronary syndrome at tertiary care hospital: a prospective cross-sectional observational study. Int J Basic Clin Pharmacol. 2016;2016(2):513-6. [CrossRef] | [Google Scholar]

- George J, Devi P, Kamath DY, Anthony N, Kunnoor NS, Sanil SS, et al. Patterns and determinants of cardiovascular drug utilization in coronary care unit patients of a tertiary care hospital. J Cardiovasc Dis Res. 2013;2013(4):214-21. [PubMed] | [CrossRef] | [Google Scholar]

- Scott IA, Heath K, Harper C, Clough A. An Australian comparison of specialist care of acute myocardial infarction. Int J Qual Health Care. 2003;2003(2):155-61. [PubMed] | [CrossRef] | [Google Scholar]

- Prabhakaran D, Jeemon P, Mohanan PP, Govindan U, Geevar Z, Chaturvedi V, et al. Management of acute coronary syndromes in secondary care settings in Kerala: impact of a quality improvement programme. Natl Med J India. 2008;2008(3):107-11. [PubMed] | [Google Scholar]

- Saju D, Joy C, Moorthy MA, Wilson B, Antony J, Singaravel S, et al. Prescription pattern and drug utilization analysis in patients with acute coronary syndrome. Indian J Pharm Pract. 2020;2020(1):73-9. [PubMed] | [Google Scholar]

- Naveen A, Sravani MR, Venkat JN. Drug utilization patterns in acute coronary syndrome at a tertiary care teaching hospital: A retrospective, non-interventional and observational study. J Pharm Innov. 2017;6(9, Part H):538 [PubMed] | [Google Scholar]

- Ravi Sankar V, Pranay KP, Raghu K, Manikanta CL, Srikanth M, Satyanarayana V, et al. Study of Various Cardiac Arrhythmias in Patients with Acute Myocardial Infarction Presenting to Emergency Department in A Tertiary Care Hospital. Indian J Emerg Med. 2020;2020(3):173-84. [PubMed] | [Google Scholar]

- Mhatre MA, Sirur FM, Rajpal DR, Shah MR. A clinical study of arrhythmias associated with acute myocardial infarction and thrombolysis. Int J Res Med Sci. 2017;2017(1):335-43. [CrossRef] | [Google Scholar]

- Shah MJ, Bhatt NR, Dabhi A, Thorat PB, Chudasama K, Patel J, et al. A study of 100 cases of arrhythmias in first week of Acute Myocardial Infarction (AMI) in Gujarat: A high risk and previously undocumented population. J Clin Diagn Res. 2014;2014(1):58-61. [PubMed] | [CrossRef] | [Google Scholar]

- Bhatia LC, Naik RH. Clinical profile of acute myocardial infarction in elderly patients. J Cardiovasc Dis Res. 2013;2013(2):107-11. [PubMed] | [CrossRef] | [Google Scholar]

- Guha S, Sethi R, Ray S, Bahl VK, Shanmugasundaram S, Kerkar P, et al. Cardiological Society of India: position statement for the management of ST elevation myocardial infarction in India. Indian Heart J. 2017;69(S1):S63-97. [PubMed] | [CrossRef] | [Google Scholar]

- Muhit MA, Rahman MO, Raihan SZ, Asaduzzaman M, Akbar MA, Sharmin N, et al. cardiovascular disease prevalence and prescription patterns at a tertiary level hospital in Bangladesh. J Appl Pharm Sci. 2012;2012(3):80-4. [PubMed] | [CrossRef] | [Google Scholar]

- Bake MA, Labu Z. Surveillance on prescribed cardiovascular drugs by generic names in Dhaka city of Bangladesh. Int J Pharm Life Sci (IJPLS). 2013;2013(4):2511-20. [PubMed] | [CrossRef] | [Google Scholar]


