Contents
ABSTRACT
Purpose
In the last decade over 17.46 million people in India died due to wrong medication and drug-drug interaction. In fact, Drug-drug interaction is the 4th leading cause of death in India. Medications used in COVID-19 management had resulted in one in five patients experiencing adverse drug reactions. Polypharmacy and self-medication are recognized as increasingly serious mortality and morbidity problem in the current healthcare system.
Materials and Methods
Pharmasure software is scripted in HTML and JavaScript. It requires very less storage space, and thus the device with less storage can perform more efficiently and effectively without any internet bugs. In this model drug interaction are included on the basis of literature and pharmaceutical journals which show dispensing and prescription errors due to drug-drug interaction. The drug interactions were studied, reviewed and scripted in the programme.
Results
Result of Pharmasure comes out as, it make easy for physician and pharmacists to check drug interactions. Pharmasure has different tabs featuring Drug interaction, Drug Food interaction, Herb Drug interaction and Pediatric dose calculation. Pharmasure is one of its kind which shows different healthcare aid at same place.
Conclusion
The Present work corroborates that harm and death due to drug-drug interaction can be prevented. People should have information of drug interaction. Pharmasure has different healthcare features on one platform.
INTRODUCTION
In last 10 years over 17.46 million people died due to wrong medication. Some adverse drug reaction are very serious cause of mortality, morbidity, Each year in India, over 2 million people are hospitalized or suffer serious injury, with over 100,000 of these incidents resulting in death. In fact, drug-drug interactions are the fourth most common cause of death in the country. Medications used in COVID-19 management had resulted that one in five patients experience adverse drug effects.
Global reports reveal that around 21% of hospital admissions due to adverse drug events are caused by drug interactions. In Australia, a study showed that approximately 100,000 cases were linked to adverse drug events, with 1.3% resulting in hospital admission.
The mortality rate is increased with the death from drug interaction. For example, deaths from an overdose of a highly active drug such as opioids, barbiturates, benzodiazepines, cocaine and amphetamines are more likely to be fatal than deaths from an overdose of a less active drug such as methadone. Death rates can also rise in conjunction with the use of more than one substance, where each one amplifies the effect on the central nervous system. This is especially risky during alcohol withdrawal.
Case-control studies as well as epidemiological studies confirm the emergency casualties due to drug interaction. Other factors that may contribute to the increase in mortality rate due to drug interaction include socioeconomic factors such as health care access, education, etc. In case-control or retrospective studies, cases are people who have died and controls are those who are alive. In the study by Monash and colleagues (1996), a control group of 27,250 people was compared to those who had died from a drug interaction.
Adverse drug reactions are a significant source of illness and death in the healthcare industry. The Institute of Medicine reported in 2000 that annually, between 44,000 and 98,000 deaths are caused by medical errors, with approximately 7,000 of these being due to adverse drug reactions.
However, other studies on hospitalized patients have found much higher numbers for the overall occurrence of serious adverse drug reactions. These studies estimate that 6.7% of hospitalized patients experience a serious adverse drug reaction, with a death rate of 0.32%. If these estimates are accurate, it would mean that there are over 2,216,000 serious adverse drug reactions among hospitalized patients each year, resulting in more than 106,000 fatalities. If this is true, then adverse drug reactions would be the fourth leading cause of death, ahead of pulmonary disease, diabetes, AIDS, pneumonia, accidents, and automobile fatalities.1–8
The reasons for the increase in adverse drug reactions include the use of more drugs and combinations of drugs in patient treatment, the filling of 2.8 billion prescriptions in 2000 (equivalent to about 10 prescriptions per person in the US), and the exponential increase in ADRs when a patient is taking four or more medications. While reducing polypharmacy is important, it is not always possible without causing harm, so understanding the causes of drug interactions is crucial to make informed decisions in prescribing and prevent preventable ADRs. It is essential to consider the level of safety defined for a drug before its approval and marketing, as this will determine the confidence of practitioners in the drug’s safety profile.
Drug-Drug Interaction
A drug interaction is reaction between two drugs. Taking medication during certain medical condition can also cause interaction with other medication. For example, taking nasal decongestant for high blood pressure may cause side effects.
The current healthcare system recognizes polypharmacy and self-medication as causes of side effects. Physician often do not know all exact amount of medication that the patient is taking and often do not check all possible interaction between both prescription and OTC drug. It is very important for every physician, pharmacist, general practitioners and family doctor, to know pharmacological action of drugs such as OTC drugs and anti-allergic drug.8–14
Food-Drug Interaction
A drug-food interaction occurs when either a food or food ingredient has an impact on the effects of a drug, or a drug affects the effects of a food or food ingredient. This can occur when drugs are taken at the same time as food or drink, or when drugs alter the way food or food components are metabolized or absorbed. Examples of drug-food interactions include: taking an antacid with an antibiotic, drinking alcohol while taking a sedative, and taking medications that affect blood sugar levels with a high-carbohydrate meal.
Food-drug interactions can cause serious health problems, such as an increased risk of hospitalization and death. One study estimated that, in the United States alone, approximately 2 million hospitalizations and 100,000 deaths are associated with adverse drug reactions that are triggered by food-drug interactions each year.
Food-drug interactions can have serious consequences, ranging from mild side effects to life-threatening reactions. In some cases, food-drug interactions can lead to hospitalization, disability,
and even death. Common side effects of drug-food interactions include symptoms such as nausea, vomiting, diarrhoea, dizziness, headaches, and other unpleasant experiences. Other serious side effects may include anaphylaxis, an allergic reaction that can be life-threatening, and Stevens-Johnson syndrome, a rare but serious skin reaction. Food-drug interactions can lead to a variety of adverse health effects, including increased risk of injury.
In severe cases, food-drug interactions can cause serious side effects. For example, consuming grapefruit juice while taking certain medications can cause an increased risk of liver damage, heart attack, or stroke. Additionally, taking certain medications with alcohol can cause seizures, coma.
Food-drug interactions can cause serious and potentially serious consequences can occur in some individuals as a result of drug-food interactions. These can include unpleasant symptoms such as nausea, vomiting, abdominal pain, damage to internal organs, and in severe cases, even death.
Herb-Drug Interactions
Herb-drug interactions refer to the interactions that occur between herbal remedies and conventional drugs. These types of interactions are more common than drug-drug interactions due to the fact that herbal medicines frequently contain multiple active ingredients, while conventional medicines typically contain only one. These interactions between herbs and drugs can lead to unexpected outcomes. For example, St. John’s wort in combination with certain anticoagulant drugs such as warfarin can amplify their effect, causing a heightened risk of bleeding. Certain herbs may also interact with other medications and alter their effectiveness. It’s essential to consult a doctor to determine if any of the herbs you are using could have an impact on your prescription medications. Herb-drug interactions have the potential to cause serious side effects, including nausea, vomiting, diarrhea, abdominal pain, headaches, dizziness, digestive issues, fatigue, skin rashes, heart rhythm problems, high blood pressure, damage to the liver or kidney, increased risk of bleeding, and interference with other medications.14–17
OBJECTIVES
- Pharmasure revive the interaction between medications and reduce the death rate and morbidity rate in human race.
- Provide a comprehensive and accurate database of drug interactions.
- It pinpoints contradictions between
- medication prescribed to a patient and others drugs, dietary supplements and food.
- Pharmasure gives the alternate remedy, Generic and Branded medicine name along with their pricing to compare the lowest.
- To find the correct dose of particular drug in pediatric patients.
- Locate to the nearest ‘Jan Aushdhi Kendra’ to get affordable medicine.
- Ensure proper warnings and notifications on potential drug interactions.
- Allow users to easily search through the database to find relevant drug interaction information.
- Include an interactive user interface that is intuitive and easy to use.
- Incorporate a range of features such as dosage information, drug brand names and generic names, and potential side effects.
- Incorporate machine learning algorithms to constantly monitor and update the drug interaction database.
- Provide an audit trail to track changes to the drug interaction database.
- Enable users to export data for further analysis.
MATERIALS AND METHODS
Pharmasure is a computer program designed to help healthcare providers and patients identify potential drug interactions. It can be employed to examine the interactions between two or more drugs, or between a drug and a food or supplement. The software is capable of providing information about drug-drug interactions, drug-food interactions, and drug-supplement interactions. It can provide warnings about potential adverse reactions from taking multiple drugs, and can even suggest alternative drugs or treatments that may be safer. In some cases, the software can also provide information about the dosage of each drug and suggest an appropriate dosing regimen.
If you take two or more medications, it’s crucial to make sure that the drugs don’t interact with each other and cause unintended side effects. But how do you know what to look for? That’s where our handy interactive Pharmasure comes in!
By simply entering the name of your medication, we will tell you everything about the potential interactions your doctor needs to know about. You’ll even be able to see which medications will work well together with your prescriptions.
Pharmasure is used to help healthcare providers and patients identify potentially dangerous drug interactions. Medications can interact with one another and cause adverse reactions, potentially resulting in severe side effects or fatalities. By using Pharmasure, healthcare providers can quickly evaluate possible drug interactions and determine which medications can be safely taken together. In addition, drug interaction checker software can also help patients better understand the potential risks of taking multiple medications and make informed decisions about their treatment.
Pharmasure is a mobile application and software. This is preliminary model which shows 2000+ drug interactions, several food drug interactions and dose calculation for the pediatric patient. It is scripted in HTML and JavaScript. This model can work on computer and laptops also. Pharmasure has different tabs featuring Drug interaction, Drug Food interaction and Pediatric dose calculation. Pharmasure is one of its kind which shows different healthcare aid at same place. As this model is offline, it has advantages over other bulky online applications. It requires very less storage space, and thus the device with less storage can perform more efficiently and effectively without any internet bugs. It has very simple, easy and convenient user interface.
In this model around 2000+ drug interaction are included on the basis of literature and pharmaceutical journals which show dispensing and prescription errors due to drug-drug interaction. The drug interactions were studied, reviewed and scripted in the programme.
Methodology
Step 1: Research and Understand Drug Interactions the first step in developing a Pharmasure is to research and understand the different types of drug interactions and the potential risks associated with them. This includes researching the different classes of drugs, their mechanisms of action, and any known interactions between them.
Step 2: Identify Data Sources: Once you have a good understanding of drug interactions, the next step is to identify data sources that can be used for the development of the Pharmasure. This includes databases of known drug interactions, as well as authoritative sources such as the FDA and the American Society of Health-System Pharmacists.
Step 3: Analyze Data Sources: Once data sources have been identified, the next step is to analyze them in order to better understand the types of drug interactions they contain and the potential risks associated with each type.
Step 4: Develop Algorithms once the data sources have been analyzed, the next step is to develop algorithms that can be used to identify potential drug interactions. This involve using HTML and JavaScript.
Step 5: Test and Validate.
Pharmasure user Interface (Figure 1)

Figure 1:
Pharmasure User Interface.
To check drug-drug Interaction (Figure 2)
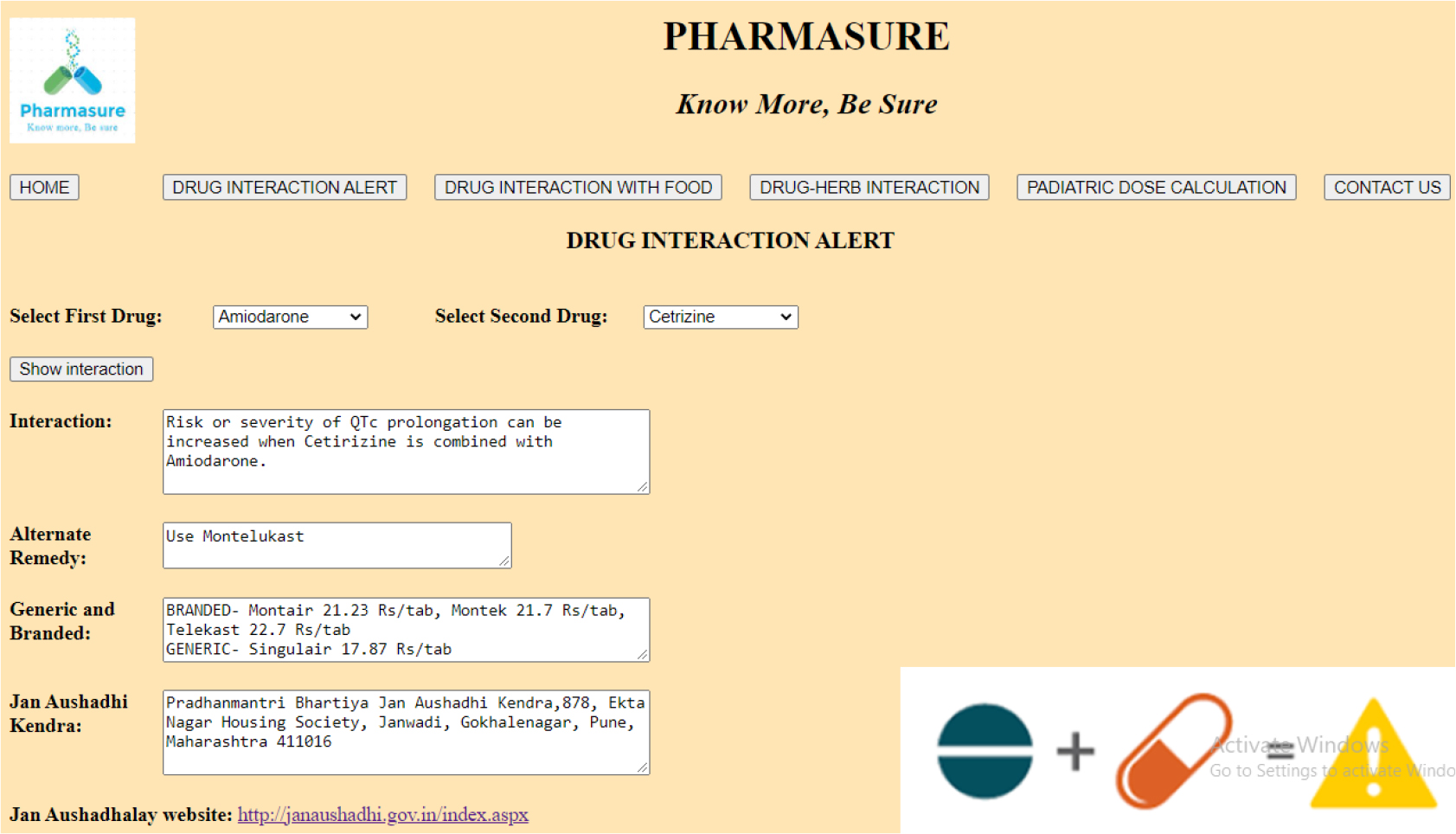
Figure 2:
Drug-Drug Interaction.
Step 1. Open Pharmasure.
Step 2. Click on “Drug Interaction Alert” button, to open Drug Interaction Alert window.
Step 3. Select first drug from given dropdown list.
Step 4. Select second drug from given dropdown list.
Step 5. Click on “Show interaction” button.
Step 6. Display interaction.
To check food drug interaction (Figure 3)
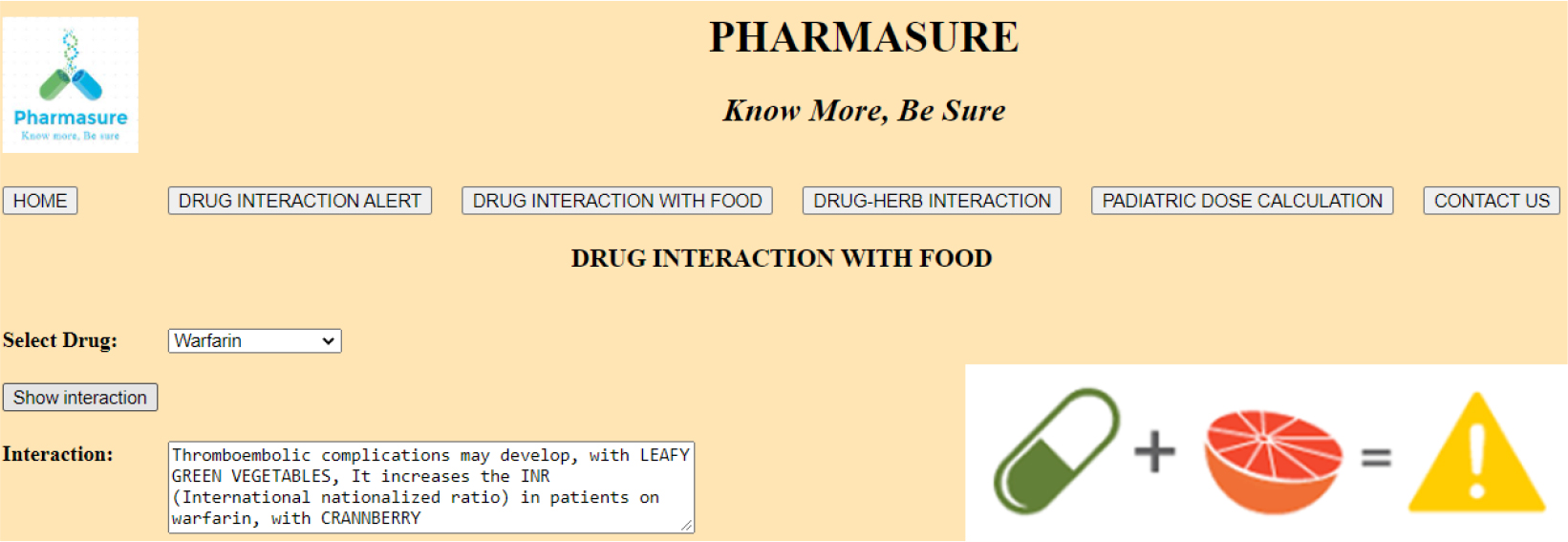
Figure 3:
Food-Drug Interaction.
Step 1. Click on “Drug interaction with food” button, to open Drug interaction with food window.
Step 2. Select drug from given dropdown list.
Step 3. Click on “Show Interaction” button.
Step 4. Display interaction.
To check herb drug interaction (Figure 4)
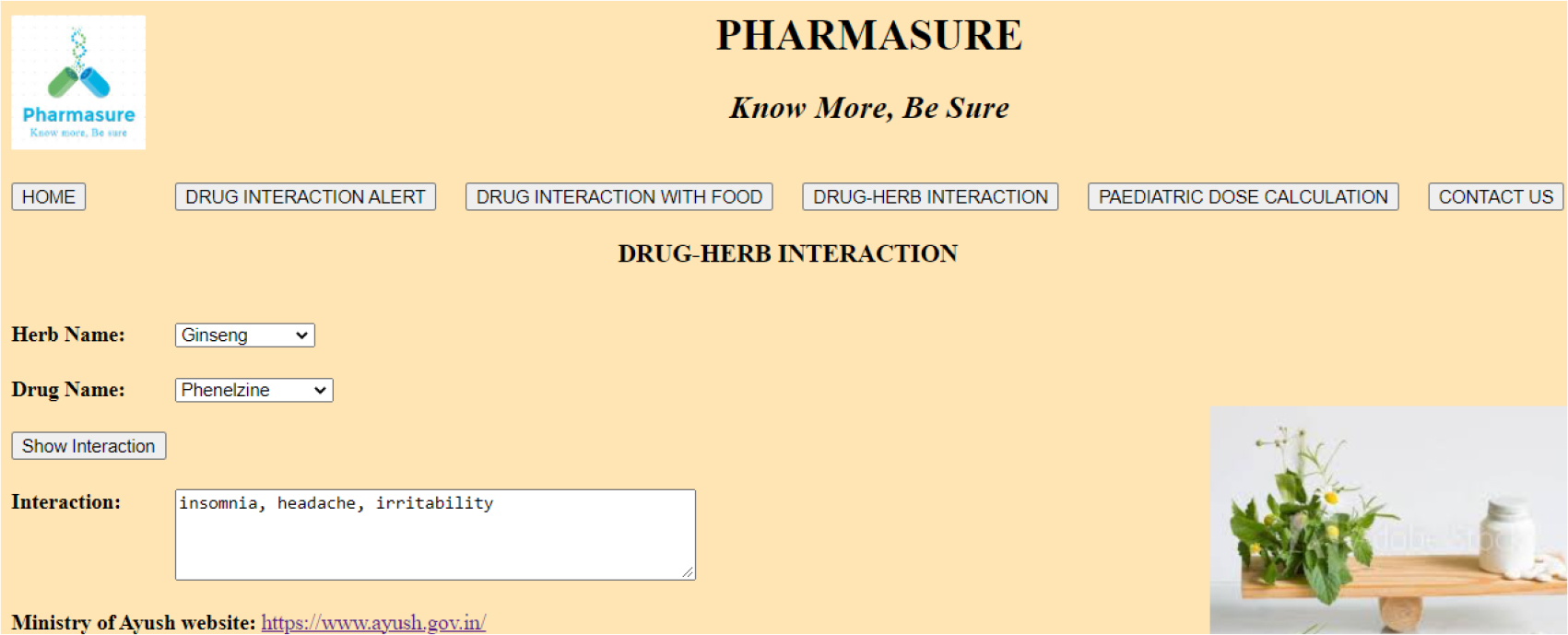
Figure 4:
Herb-Drug Interaction.
Step 1. Click on “Drug-herb Interaction” button, to open Drug-herb Interaction window.
Step 2. Select herb from given dropdown list.
Step 3. Select drug from given dropdown list.
Step 4. Click on “Show Interaction” button.
Step 5. Display interaction.
To calculate pediatric dose (Figure 5)
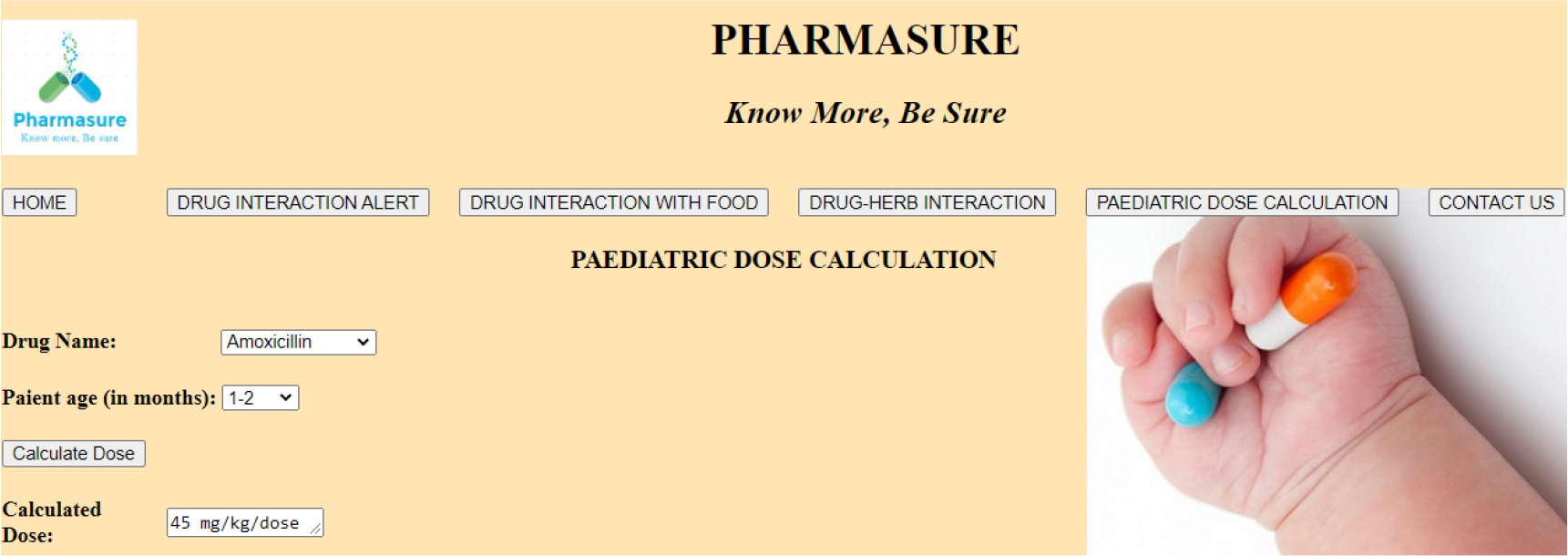
Figure 5:
Pediatric Dose Calcutaion.
Step 1. Click on “Pediatric Dose calculation” button, to open Pediatric dose calculation window.
Step 2. Select drug from given dropdown list.
Step 3. Select patient age (in months) from given dropdown list.
Step 4. Click on “Calculate Dose” button.
Step 5. Display calculated dose.
RESULTS AND DISCUSSION
Increased awareness of drug interactions: Pharmasure software can alert healthcare providers to potential drug interactions and help them make more informed decisions about prescribing medications. This can reduce the risk of adverse drug events and help improve patient outcomes.
Improved patient safety: By informing healthcare providers of potential drug interactions, food-drug interactions and herb-drug interactions can help minimize the likelihood of medication mistakes and other negative outcomes. This can save lives and improve patient safety.
Enhanced patient communication: Pharmasure can provide a platform for healthcare professionals to communicate with patients about the potential risks of drug interactions. This can help improve patient understanding, compliance, and adherence to prescribed treatments.
Cost savings: By reducing the risk of adverse drug events, Pharmasure can help to reduce healthcare costs. This can help healthcare providers save money and reinvest it into other areas of patient care. As it gives generic option along with its price, and locates to nearest ‘Jan Aushdhi Kendra’ to get medicine at affordable price.
Improved safety: Pharmasure can help healthcare professionals and patients identify potential drug interactions and adverse reactions before prescriptions are filled. This reduces the risk of dangerous side effects or complications from taking multiple medications.
Increased efficiency: Pharmasure can quickly and accurately assess the potential for drug interactions and adverse reactions. This reduces the time spent by healthcare professionals and patients in evaluating potential drug interactions and can significantly improve the overall efficiency of the healthcare system.
Reduced errors: Pharmasure software can help reduce prescribing errors by alerting healthcare professionals of potential drug interactions before prescriptions are filled. This can reduce the risk of serious health complications and improve patient safety.
Simplified Documentation: Pharmasure software simplifies the process of documenting drug interactions and can help to ensure that all interactions are properly documented. This can help to ensure that patient records are accurate and up-to-date.
CONCLUSION
This study supports the notion that harm and death caused by drug-to-drug interactions can be prevented. It’s important for individuals to have a good understanding of drug interactions before taking any medications, especially if they are taking multiple drugs at the same time. There are many drugs that commonly result in interactions, and the harmful effects of these interactions are also discussed. Drug-to-drug interactions are a common problem in patients who are taking multiple drugs, and even just two drugs can interact. The study found that age is a factor in drug interactions, with those under 18 being less likely to experience these interactions, and that taking multiple drugs (polypharmacy) can also increase the risk of drug-to-drug interactions. Pharmasure software is a valuable tool for healthcare providers, pharmacists, and patients alike. It can help identify potential drug interactions, provide patient education and help improve medication safety. It can also help to reduce medication errors, which can lead to serious harm.
Pharmasure is useful tool for medical professionals and patients alike. It can help them identify potential drug interactions and reducing the risk of adverse drug reactions. It also allows patients to become more informed and proactive in their healthcare decisions. By reducing the risks associated with drug interactions, the potential for harm is minimized and quality of care is improved. It helps to ensure safe medication use by providing important information interactions. The software can also provide helpful information on dosages, side effects, and other important drug-related information. With Pharmasure’s aid, the likelihood of serious drug interactions can be greatly reduced and the quality of care improved.17–23
Future Scope
This technology can be modified into handy application and more drugs can be added into it. More specific option such as route of administration and dose amount. The knowledge about food-drug interaction may helpful to reduce uncertain problem, health problems and sometimes severe harms.
This technology can be modified by adding more specific option such as route of administration, dose amount and remedy for interaction can be amended. This app can be linked with the billing software, by entering the items in bill it will automatically check the interactions and if incase found one then it will give alert to stop dispensing.
References
- Zhang L, Reynolds KS, Zhao P, Huang SM. Drug-drug interactions: a review and assessment of tools. Mol Pharm.. 2010;7(3):594-612. [Google Scholar]
- Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998;279(15):1200-5. [PubMed] | [CrossRef] | [Google Scholar]
- Nair AB, Jacob S.. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm.. 2016;7(2):27-31. [PubMed] | [CrossRef] | [Google Scholar]
- Wu L, Tran N, Danks R, Lee E, Fang J, Lee C., et al. Evaluation of a clinical decision support system for drug-drug interaction alerts in outpatient setting: a study protocol for a randomized controlled trial. Trials. 2017;18(1):85 [PubMed] | [CrossRef] | [Google Scholar]
- Ge Y, Zhang X, Chen Y, Cao Y.. A review of computer-based decision support systems for drug-drug interactions. J Med Syst. 2020;44(9):1-13. [PubMed] | [CrossRef] | [Google Scholar]
- Lin JC, Hu YH. A review of current applications of computer-based decision support systems for drug-drug interactions. Expert Opin Drug Saf.. 2019;18(6):453-66. [PubMed] | [CrossRef] | [Google Scholar]
- Nevo I, Finkelstein I, Aharonson-Daniel L. Evaluation of computerized drug-drug interaction detection systems for improved patient safety. Int J Med Inform.. 2019;129:289-97. [PubMed] | [CrossRef] | [Google Scholar]
- Bouvy JC, Herings RM, Klungel OH, de Bruin ML, De Boer A.. Use of outpatient pharmacy data for pharmacoepidemiologic research. J Clin Epidemiol. 2001;54(2):193-201. [PubMed] | [CrossRef] | [Google Scholar]
- Patel H, Bell D, Molokhia M, Srishanmuganathan J, Patel M, Car J, et al. Trends in hospital admissions for adverse drug reactions in England: analysis of national hospital episode statistics 1998-2005. BMC Clin Pharmacol. 2015;15(1):11 [PubMed] | [CrossRef] | [Google Scholar]
- Rastegar-Mojarad M, Ye Z, Kolesar JM, Hebbring SJ, Lin SM. Opportunities for drug repositioning from phenome-wide association studies. Nat Biotechnol. 2015;33(4):342-5. [PubMed] | [CrossRef] | [Google Scholar]
- Malone DC, Hutchins DS, Haupert H, Hansten P, Duncan B, Van Bergen RC, et al. Assessment of potential drug interactions with a prescription claims database. Ann Pharmacother. 2004;38(5):839-44. [PubMed] | [CrossRef] | [Google Scholar]
- Shah RR. Importance of publishing adverse drug reaction case reports: promoting public health and advancing pharmacology and therapeutics. Drug Saf Case Rep.. 2017;4(1):11 [PubMed] | [CrossRef] | [Google Scholar]
- Weathermon R, Crabb DW. Alcohol and medication interactions. Alcohol Res Health. 1999;23(1):40-54. [PubMed] | [Google Scholar]
- Uhart M, Wand GS. Stress, alcohol and drug interaction: an update of human research. Addict Biol. 2009;14(1):43-64. [PubMed] | [CrossRef] | [Google Scholar]
- Magro L, Moretti U, Leone R. Epidemiology and characteristics of adverse drug reactions caused by drug-drug interactions. Expert Opin Drug Saf.. 2012;11(1):83-94. [PubMed] | [CrossRef] | [Google Scholar]
- Moore N.. The role of the clinical pharmacologist in the management of adverse drug reactions. Drug Saf. 2001;24(1):1-7. [PubMed] | [CrossRef] | [Google Scholar]
- Gollnick H, Schramm M.. Topical drug treatment in acne. Dermatology. 1998;196(1):119-25. [PubMed] | [CrossRef] | [Google Scholar]
- Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol.. 2006;54(1):1-15. [PubMed] | [CrossRef] | [Google Scholar]
- Zinsstag J, Schelling E, Waltner-Toews D, Tanner M.. From “one medicine” to “one health” and systemic approaches to health and well-being. Prev Vet Med.. 2011;101(3-4):148-56. [PubMed] | [CrossRef] | [Google Scholar]
- Ungemach FR, Müller-Bahrdt D, Abraham G. Guidelines for prudent use of antimicrobials and their implications on antibiotic usage in veterinary medicine. Int J Med Microbiol. 2006;296(Suppl 41):33-8. [PubMed] | [CrossRef] | [Google Scholar]
- Chi LH, Burrows AD Anderson RL. Can preclinical drug development help to predict adverse events in clinical trials?. Drug Discov Today.. 2022;27(1):257-68. [PubMed] | [CrossRef] | [Google Scholar]
- Clancy CM. New patient safety organizations can help health providers learn from and reduce patient safety events. J Patient Saf. 2009;5(1):1-2. [PubMed] | [CrossRef] | [Google Scholar]
- Abdelaziz I, Fokoue A, Hassanzadeh O, Zhang P, Sadoghi M.. Large-scale structural and textual similarity-based mining of knowledge graph to predict drug-drug interactions. J Web Semant. 2017;44:104-17. [CrossRef] | [Google Scholar]
