Contents
ABSTRACT
Background
Postpartum Depression (PPD) is one of the least vocalized topics surrounding pregnancy and motherhood in India. The study aimed to assess the postpartum depression in women who had cesarean and normal vaginal deliveries.
Materials and Methods
In this study, we identify postpartum depression in recently postpartum women and compare it in different maternal ages, modes of delivery (cesarean and vaginal), and sexes of the babies, since very few studies have explored these as risk factors. Data were obtained over six months from 210 women via their responses to the Edinburgh Postnatal Depression Scale (EPDS). An EPDS score of ≥7 out of 30 was set to determine postpartum depression, which was further classified as mild, moderate, or severe.
Results
Total of 210 patients analyzed in the study out of which 157 (74.7%) exhibited PPD, which was more common in mothers aged between 19 and 27 years, and those who delivered via cesarean section. Mild depression was the most frequently occurring severity overall.
Conclusion
Screening of PPD and providing suitable education should be encouraged during postpartum care or child-care visits for identifying and managing PPD, which in turn improves child development.
INTRODUCTION
Postpartum Depression (PPD) is one of the least talked about conditions in a woman’s pregnancy journey in India. It is a major depressive disorder that occurs within the first four weeks after delivery and can extend up to a year postpartum. In some, depression may begin during pregnancy itself.1,2 The social stigma associated with depression often hinders new mothers from getting professional assistance.3 Women with PPD face intense emotional and psychological changes that may affect their ability to cope with stressors and bond with their newborns.4
Since the 1970s, cesarean birth was linked to negative psychological effects on women.5,6 Some studies have shown that a delivery needing an emergency operation is more likely to cause PPD,7–10 whereas others have shown no link between the mode of delivery and depression.10–14 Unplanned pregnancies, unplanned modes of delivery, and unfavorable childbirth experiences can also result in increased anxiety and stress, leading to postpartum depression in newly delivered women. Severe pain and discomfort after a cesarean section delivery also contribute to further stress.12,15–24 Reviews of the psychological effects of a cesarean section have either (1) failed to distinguish between studies looking at PPD and those looking at other psychological outcomes or (2) have reached contradictory findings.25–27
Data have also not identified whether the mother’s age is a risk factor for PPD or not. People often believe that young mothers have an increased risk for depressive symptoms after delivery owing to their lesser knowledge about pregnancy, delivery, baby care, and self-care.11,14,28–30 Conversely, women who marry at late ages, or have late pregnancies may also suffer a lot from stress and experience low mood as well. Some studies also speculate that the gender of the child may increase the likelihood of PPD.30–32
Around 10-20% of women worldwide experience PPD. However, the actual estimate probably lies higher, due to the lack of regular screening in pregnant and postnatal women and/or their reluctance to admit to having depressive thoughts and feelings. One way of properly providing care for women affected by PPD is to identify the predisposing factors. Therefore, it is necessary to research postpartum depression and its potential risk factors, to help healthcare professionals detect and manage it successfully.
We hypothesize that PPD would be a more frequent occurrence in women who delivered via a cesarean section, and in those of a relatively young age; women with a girl child may have a higher likelihood, especially in the lower socioeconomic sector of India. The EPDS (Edinburgh Postnatal Depression Scale)-an accurate scale developed by Cox et al.-was used to identify women with depression. Cox et al. designate mothers with a score of 13 and above as ‘depressed with varying severity’, and ten and above as ‘possibly depressed’. In this study, we examined postpartum depression in women who have undergone recent deliveries in a prominent hospital in India, and compared it in cesarean and vaginal modes of delivery, the women’s age groups, and the gender of the baby. We decided that the cut-off score for depression be set as seven and above; scores seven to thirteen indicate ‘mild depression’ and may largely entail postpartum baby blues, which is the milder and briefer form of PPD.
MATERIALS AND METHODS
Study Design
The research employs a prospective, observational design. We approached women admitted post-delivery in the Obstetrics and Gynecology department at Vivekananda General Hospital, Hubli. We reviewed the case files for patients’ demographic details, medical and surgical history, medication history, and mode of delivery details. All women who had given birth, vaginally or via C-section, within the prior week were considered. After obtaining their consent for their participation in this study, we enquired about their delivery experience, their postpartum moods and outlooks, and their sleeping and eating patterns. Verbal responses to the EPDS (Edinburgh Postnatal Depression Scale) questions were noted down. The participants were assessed and data were collected for six months. The individual scores were then counted, based on which, the women were categorized as having no, mild, moderate, or severe depression. The occurrence of PPD was analyzed with respect to the mode of delivery, maternal age, and the gender of the infant.
Study Setting
We conducted the research in Hubli, a city in the south Indian state of Karnataka. Hubli along with its twin city Dharwad is the second largest city in Karnataka. The study took place in Vivekananda General Hospital, a multispecialty hospital with 150 beds; it is one of the most prominent and renowned hospitals in the city.
Measures
The EPDS is an accurate scale used for the detection of postpartum depression developed by Cox et al. It is a ten-item questionnaire, with the answers rated from zero to three. The questions specifically reflect the mood of the mother in the past week. The EPDS, however, does not override the clinical diagnosis, nor is it used as a diagnostic tool.
The maximum score one can obtain is 30. We characterize the EPDS scores of 7 and above as depression; it was further categorized into mild, moderate, and severe depression. The severity was established according to the following scores:
No depression: 0-6,
Mild depression: 7-13,
Moderate depression: 14-19,
Severe depression: 20-30.33
Sampling and Data Collection
For this research, we approached women who had delivered within one week and were present in the Obstetrics and Gynecology department of the hospital. We included all women who had given birth vaginally or via C-section, preterm and full-term deliveries, and premenopausal and postmenopausal women. The cesarean deliveries included elective and emergency deliveries. Data were collected for six months, from November 2021 to April 2022. We obtained all the relevant data from the women’s hospital files and their verbal answers to the face-to-face questioning; these data were later fed into a Microsoft Excel sheet. A total of 250 questionnaires were administered to the eligible women over the research period of six months. 216 answered; 34 women denied providing details. Complete data were available for 210 women and their responses were examined.
RESULTS
Over six months, 250 questionnaires were distributed to the eligible women, and 210 of those that chose to participate had complete data. Most participants came from a relatively lower socioeconomic background.
The EPDS scores of the participants ranged from 0 to 22. We identified 157 out of 210 women with depression (EPDS scores ≥7), accounting for 74.7% of all women; a quarter presented no postpartum depressive symptoms (Figure 1). Mild depression was the most common severity of PPD, affecting two-thirds of all depressed women (Figure 2).
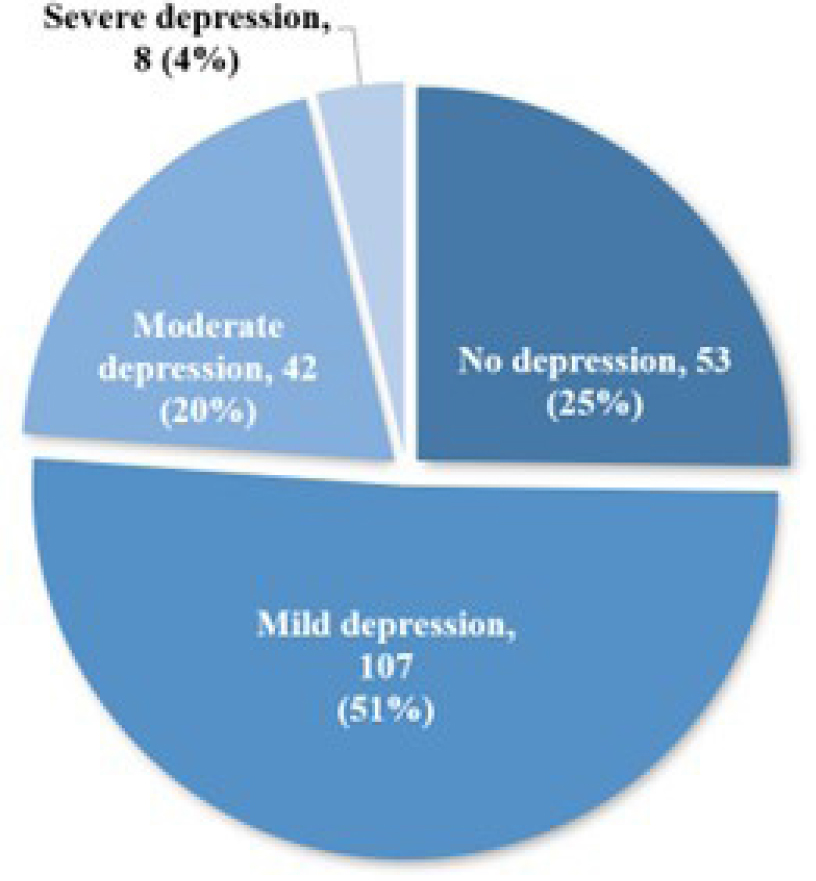
Figure 1:
Incidence of Postpartum Depression.
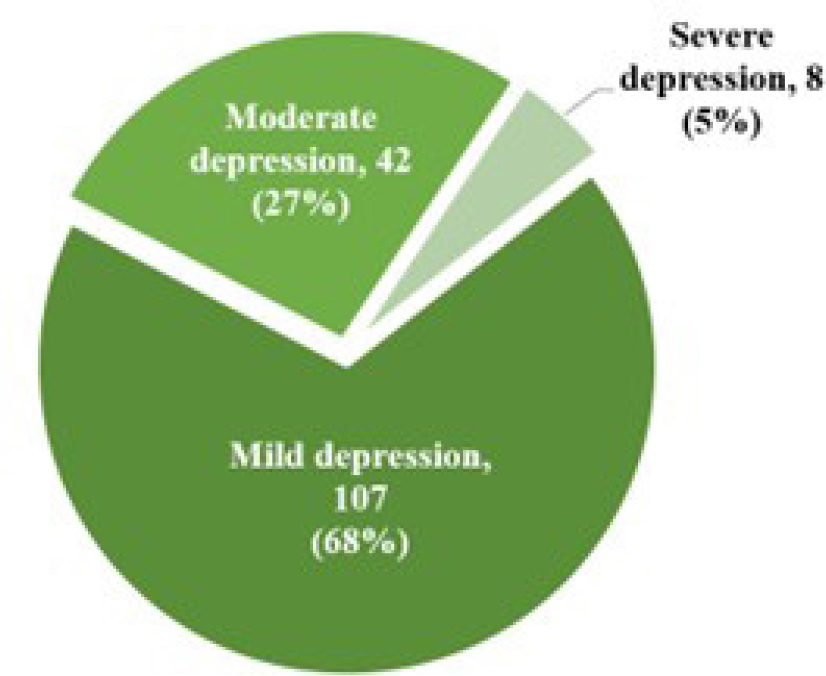
Figure 2:
Distribution of Postpartum depression according to the severity.
Postpartum Depression and Mode of Delivery
Most women had given birth via a C-section (Lower-Segment Cesarean Section, LSCS) (Table 1). The majority of the 157 depressed women underwent an LSCS (60%) whereas the rest (40%) had a Normal Vaginal Delivery (NVD) (Table 1). PPD occurred in 77% of the LSCS-delivered women and 72% of the NVD-delivered population. Figure 3 illustrates the distribution of depression by the mode of delivery.
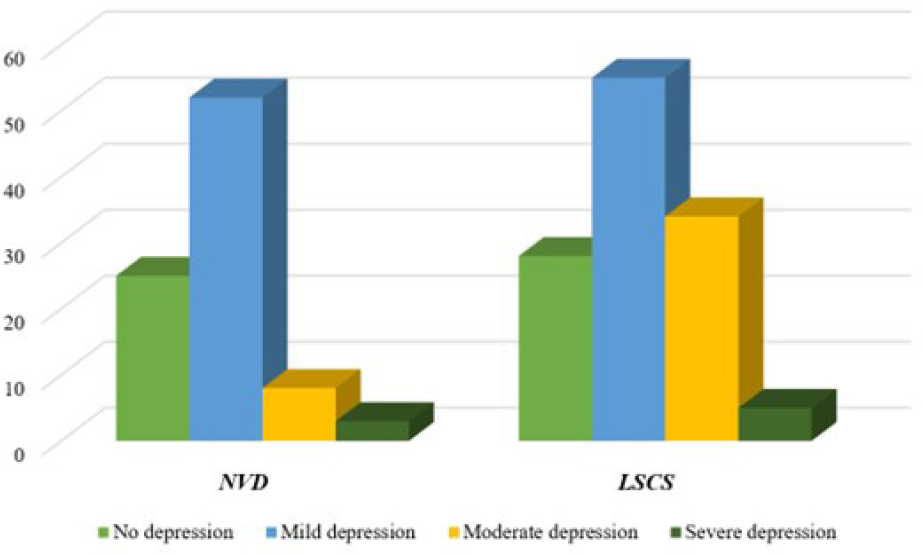
Figure 3:
Distribution of PPD and its severity in the two modes of delivery.
| Non-Depressed | Depressed | Total | ||||
|---|---|---|---|---|---|---|
| Mild depression | Moderate depression | Severe depression | ||||
| Mode of Delivery | NVD | 25 | 52 | 8 | 3 | 88 |
| 63 | ||||||
| LSCS | 28 | 55 | 34 | 5 | 122 | |
| 94 | ||||||
| Total | 53 | 107 | 42 | 8 | 210 | |
| Age | 19-22 yrs | 24 | 33 | 27 | 6 | 90 |
| 66 | ||||||
| 23-27 yrs | 21 | 55 | 11 | 2 | 89 | |
| 68 | ||||||
| 28-33 yrs | 8 | 19 | 4 | 0 | 31 | |
| 23 | ||||||
| Total | 53 | 107 | 42 | 8 | 210 | |
| Gender | BOY | 18 | 55 | 12 | 2 | 87 |
| 69 | ||||||
| GIRL | 35 | 52 | 30 | 6 | 123 | |
| 88 | ||||||
| Total | 53 | 107 | 42 | 8 | 210 | |
Postpartum Depression and Maternal Age
Participants in the study participants ranged in age from 19 to 33 years old. We categorized them into three age groups: lower age group (19-22 years), median age group (23-27 years), and higher age group (28-33 years). Most women belonged to the lower and median age groups (Table 1). Most depressed women were younger as well; the lower and median age groups comprised 42% and 43%, respectively, while the higher age group included only 15% (Table 1). Mild depression was the most predominant type seen across all groups, especially in the median age group. About a quarter of each age group showed no signs of PPD (Figure 4).
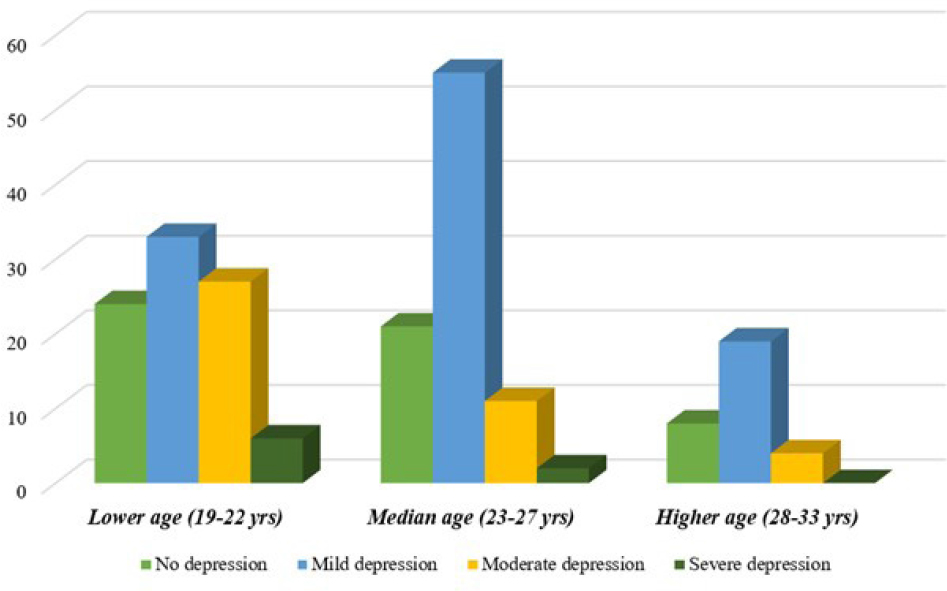
Figure 4:
Distribution of PPD and its severity in different maternal ages.
Postpartum Depression and Gender of the Baby
Our findings revealed that more women had given birth to a baby girl than a baby boy (Table 1). However, we detected depression in 79.3% of women with male babies and 71.5% of women with female babies. Mild depression again affected most of the women in each group (Figure 5). The high proportion of mild depression in the former group is mostly responsible for the larger number of depressed women in that group.
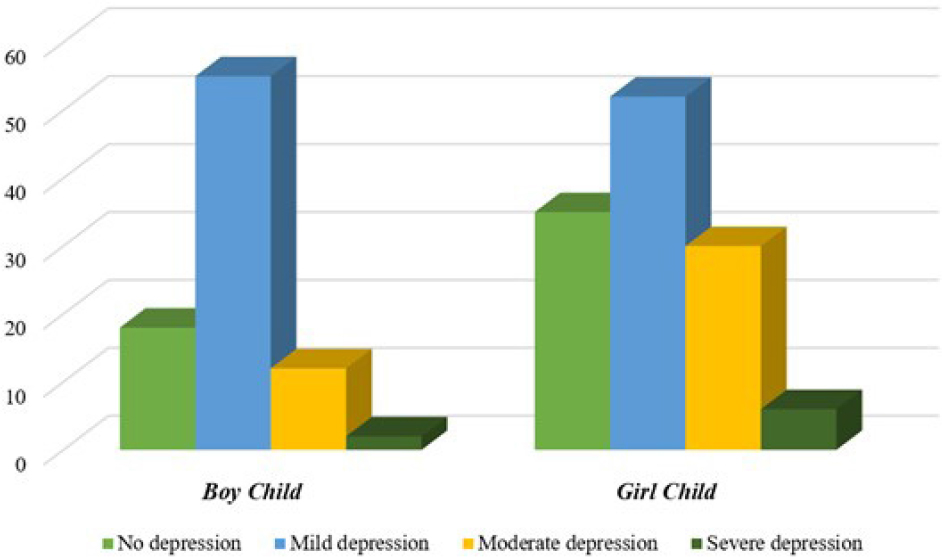
Figure 5:
Distribution of PPD and its severity in mothers with boy and girl babies.
DISCUSSION
We found that Postpartum Depression (PPD) was more common in younger mothers between 18 and 27 years of age, in cesarean-delivered women, and in those who gave birth to a male baby. Mild depression outweighed moderate and severe depression, comprising two-thirds of all depressed cases.
PPD affects around 10-20% of new mothers worldwide, with variations in different parts of the world. Upadhyay R P et al. (2017) reported an overall prevalence of 22% in Indian women, and 19% when considering depression solely after two weeks postpartum.34 According to Ostacoli L et al. (2020), during the Covid-19 pandemic, 44.2% of women in Italy suffered from PPD (EPDS ≥11).35 In Portugal, 25.9% of adolescent mothers and 9.3% of adult mothers presented with PPD, as studied by Figueiredo B et al.36 A review by Klainin P et al. (2009) revealed that PPD prevalence ranged from 3.5% to 63.3% across 17 different Asian countries.37 In another study conducted in India, in the state of Gujarat, PPD was 48.5% prevalent (EPDS ≥10.5).38 In our research, PPD was seen in 74.7% of the participants with a cut-off score of EPDS ≥7; almost two-thirds (60%) of the depressed women had undergone a C-section (LSCS).
Women that undergo a cesarean section recover more slowly and often report a negative delivery experience including increased psychological stress, somatic complaints, and more hospitalization. Due to sociocultural beliefs, a C-section is often seen as undesirable, and having one comes with low self-esteem, lack of social support, a feeling of disappointment or loss of control, and a sense of failure for not being able to conceive vaginally. It has a social stigma attached to it in many cultures, making it an undesirable option for delivery. Severe pain and discomfort following a cesarean section delivery also add to further stress.12,15–24 Meky H K et al. (2019) similarly compared PPD (EPDS ≥13) in women who delivered vaginally or via a C-section (elective and emergency). At 8 and 16 weeks postpartum, the mode of delivery showed a strong association with PPD, with emergency C-sections being more likely than elective C-sections.39
However, some studies suggest PPD is not directly influenced by complications during pregnancy and delivery.4,40,41 Women who experience complications during delivery may also be at a lower risk of PPD because they receive better and more intensive care.4 Research such as those done by Eckerdal P et al. (2018) in Uppsala, Sweden, and by Sword W et al. (2011) implied that the mode of delivery itself did not directly influence PPD, but the unfavorable childbirth experiences associated with an emergency C-section or a vacuum extraction delivery may predispose women to it.28,42
A woman’s initial expectations of their delivery experience are more relevant than the mode of delivery itself.42 According to Houston K A et al. (2014), women who highly preferred vaginal birth before delivery but subsequently have a C-section tend to be at a higher risk for PPD.43
PPD is also strongly linked to maternal age, with younger mothers being especially more vulnerable. Among the women that participated in this study, ranging from 19 to 33 years of age, most who were identified as depressed were on the younger side. Many studies conclude that young maternal age is related to a higher risk of PPD, especially when additional risk factors are also present.8,28–30,44 Petrosyan D et al. (2011) reported that women under the age of 25 who had a cesarean section had a greater risk of PPD than those who underwent a normal delivery.8 According to Doi S et al. (2019), younger mothers are not only more likely to present with PPD but also with postpartum suicidal ideation, with a 10.3-fold increase in those who had a traumatic upbringing.44 Adolescents are more affected by depression during pregnancy and postpartum and display significantly higher suicide rates.45,46 Younger mothers are usually first-time mothers. Inexperience combined with an unplanned mode of delivery, unfavorable childbirth experiences, and familial and societal pressures can result in increased anxiety and stress, leading to postpartum depression.
We also found that women who birthed a female infant exhibited a comparable post-delivery depression percentage, compared with those who had a male infant. Excluding mild depression, the majority of the depressed were girl mothers. In India, especially in the rural sectors, a newborn girl has traditionally been seen as undesirable.30–32,47 However, some studies report that mothers of newborn boys have depressive symptoms and reduced quality of life compared to mothers of newborn girls.48,49 Seeing the child’s gender as undesirable may have a measurable influence on the development of PPD.50
Our research largely included women belonging to the lower socioeconomic class, which may explain the high frequency of postpartum depression. Underprivileged women experience exacerbated financial difficulties after the birth of a child. They may have limited resources to accommodate the new changes that come with a newborn, in addition to day-to-day stressors like inadequate pay, food, and transportation. Unplanned pregnancies, even if welcome, come with unexpected and sudden changes that the mother must cope with. As a result, increased stress and decreased coping strategies can precipitate depression, which can further hinder their ability to work their way out of poverty.3,51
We set an EPDS cut-off score of 7 and above to determine PPD.33 Most of the research utilizing the EPDS questionnaire employs the suggested cut-off score by Cox: 13 and above suggesting depression and 10 and above suggesting possible depression. Setting a lower cut-off score declares a greater number of women affected. Our findings also revealed mild depression (EPDS score 7-13) as the most common severity of PPD. Mild depression, in this context, may also include cases of postpartum baby blues-a milder, briefer version of PPD that occurs within the first ten days of delivery and can persist for up to two weeks. Fifty to eighty-five percent of postpartum women experience baby blues, which may also explain the high occurrence seen in this study.52–59 If we were to consider only women with EPDS scores above 13, the total number of women depressed would be only 50, i.e., 24% of all new mothers. This study might also be possibly influenced by different biases. Because of the acquiescence bias, participants may have agreed in experiencing the symptoms; interviewer bias may also have influenced responses.
CONCLUSION
Screening can be encouraged during postpartum health-care visits or child-care visits. Antenatal screening is also important for detecting symptoms and triggers early on, and proper care can further prevent recurrent PPD. Suicidal ideation is also more prevalent in women who abuse substances or have psychiatric disorders. Thus, suicidality should be examined during screening, focusing on a history of substance abuse, psychiatric illness, previous trauma, previous suicide attempts, and intimate partner violence.
PPD can be prevented to a degree by interpersonal psychotherapy, counseling, and guidance in family planning. Before and after delivery, women should be educated about the pregnancy process, the different modes of delivery and their potential complications, and against false superstitions regarding the gender of the baby. More research on postpartum depression and its potential risk factors can bring about awareness and positive changes in its perception as well as improve postpartum screening and care.
Cite this article:
Nyamagoud SB, Swamy AHV, Fernandes L, Kanavi RS, Sultana S, Alex AA. Assessment of Postpartum Depression in Women who had Cesarean and Normal Vaginal Deliveries. Int. J. Pharm. Investigation. 2024;14(1):165-71.
ACKNOWLEDGEMENT
The authors are thankful to the Vice-Chancellor, Registrar and Dean of Pharmacy, KLE Academy of Higher Education and Research, Belagavi. We would also like to thank Medical and Hospital Staff of Vivekanand General Hospital, Hubballi for providing necessary support.
ABBREVIATIONS
| COVID-19 | Coronavirus disease-2019 |
|---|---|
| C-section | Cesarean section |
| DSM-5 | Diagnostic and Statistical Manual of Mental Disorders, fifth edition |
| EPDS | Edinburgh Postnatal Depression Scale |
| LSCS | Lower segment cesarean section |
| NVD | Normal vaginal delivery |
| PPD | Postpartum depression |
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 2000
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T, et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106((5 Pt 1)):1071-83. [PubMed] | [CrossRef] | [Google Scholar]
- Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50(5):275-85. [PubMed] | [CrossRef] | [Google Scholar]
- Paykel ES, Emms EM, Fletcher J, Rassaby ES. Life events and social support in puerperal depression. Br J Psychiatry. 1980;136(4):339-46. [PubMed] | [CrossRef] | [Google Scholar]
- Bradley C. The effects of hospital experience on postpartum feelings and attitudes of women. 1977 [PubMed] | [CrossRef] | [Google Scholar]
- Cohen NW. Minimizing emotional sequelae of caesarean childbirth. Birth. 1977;4(3):114-9. [CrossRef] | [Google Scholar]
- Goecke TW, Voigt F, Faschingbauer F, Spangler G, Beckmann MW, Beetz A, et al. The association of prenatal attachment and perinatal factors with pre- and postpartum depression in first-time mothers. Arch Gynecol Obstet. 2012;286(2):309-16. [PubMed] | [CrossRef] | [Google Scholar]
- Petrosyan D, Armenian HK, Arzoumanian K. Interaction of maternal age and mode of delivery in the development of postpartum depression in Yerevan, Armenia. J Affect Disord. 2011;135((1-3)):77-81. [PubMed] | [CrossRef] | [Google Scholar]
- Boyce PM, Todd AL. Increased risk of postnatal depression after emergency caesarean section. Med J Aust. 1992;157(3):172-4. [PubMed] | [CrossRef] | [Google Scholar]
- Koo V, Lynch J, Cooper S. Risk of postnatal depression after emergency delivery. J Obstet Gynaecol Res. 2003;29(4):246-50. [PubMed] | [CrossRef] | [Google Scholar]
- McCoy SJB, Beal JM, Saunders B, Hill EN, Payton ME, Watson GH, et al. Risk factors for postpartum depression: a retrospective investigation. J Reprod Med. 2008;53(3):166-70. [PubMed] | [Google Scholar]
- Wiklund I, Edman G, Andolf E. Cesarean section on maternal request: reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstet Gynecol Scand. 2007;86(4):451-6. [PubMed] | [CrossRef] | [Google Scholar]
- Carter FA, Frampton CM, Mulder RT. Cesarean section and postpartum depression: a review of the evidence examining the link. Psychosom Med. 2006;68(2):321-30. [PubMed] | [CrossRef] | [Google Scholar]
- Goker A, Yanikkerem E, Demet MM, Dikayak S, Yildirim Y, Koyuncu FM, et al. Postpartum depression: is mode of delivery a risk factor?. ISRN Obstet Gynecol. 2012;2012 [PubMed] | [CrossRef] | [Google Scholar]
- Ryding EL, Wijma B, Wijma K, Rydhström H. Fear of childbirth during pregnancy may increase the risk of emergency cesarean section. Acta Obstet Gynecol Scand. 1998;77(5):542-7. [PubMed] | [CrossRef] | [Google Scholar]
- Waldenström U, Hildingsson I, Ryding EL. Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG. 2006;113(6):638-46. [PubMed] | [CrossRef] | [Google Scholar]
- Laursen M, Johansen C, Hedegaard M. Fear of childbirth and risk for birth complications in nulliparous women in the Danish National Birth Cohort. BJOG. 2009;116(10):1350-5. [PubMed] | [CrossRef] | [Google Scholar]
- Ryding EL, Wirfelt E, Wängborg IB, Sjögren B, Edman G. Personality and fear of childbirth. Acta Obstet Gynecol Scand. 2007;86(7):814-20. [PubMed] | [CrossRef] | [Google Scholar]
- Ryding EL, Lukasse M, Van Parys AS, Wangel AM, Karro H, Kristjansdottir H, et al. Fear of childbirth and risk of cesarean delivery: a cohort study in six European countries. Birth. 2015;42(1):48-55. [PubMed] | [CrossRef] | [Google Scholar]
- Johnson R, Slade P. Does fear of childbirth during pregnancy predict emergency caesarean section? BJOG. Array. 2002;109(11):1213-21. [PubMed] | [CrossRef] | [Google Scholar]
- Weisman O, Granat A, Gilboa-Schechtman E, Singer M, Gordon I, Azulay H, et al. The experience of labor, maternal perception of the infant, and the mother’s postpartum mood in a low-risk community cohort. Arch Womens Ment Health. 2010;13(6):505-13. [PubMed] | [CrossRef] | [Google Scholar]
- Gürber S, Bielinski-Blattmann D, Lemola S, Jaussi C, von Wyl A, Surbek D, et al. Maternal mental health in the first 3-week postpartum: the impact of caregiver support and the subjective experience of childbirth – a longitudinal path model. J Psychosom Obstet Gynaecol. 2012;33(4):176-84. [PubMed] | [CrossRef] | [Google Scholar]
- Bell AF, Carter CS, Davis JM, Golding J, Adejumo O, Pyra M, et al. Childbirth and symptoms of postpartum depression and anxiety: a prospective birth cohort study. Arch Womens Ment Health. 2016;19(2):219-27. [PubMed] | [CrossRef] | [Google Scholar]
- Fairbrother N, Woody SR. Fear of childbirth and obstetrical events as predictors of postnatal symptoms of depression and post-traumatic stress disorder. J Psychosom Obstet Gynaecol. 2007;28(4):239-42. [PubMed] | [CrossRef] | [Google Scholar]
- Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993;37(10):1271-81. [PubMed] | [CrossRef] | [Google Scholar]
- Clement S. Psychological aspects of caesarean section. Best Pract Res Clin Obstet Gynaecol. 2001;15(1):109-26. [PubMed] | [CrossRef] | [Google Scholar]
- Fisher JRW, Stanley RO, Burrows GD. Psychological adjustment to Caesarean delivery: a review of the evidence. J Psychosom Obstet Gynecol. 1990;11(2):91-106. [CrossRef] | [Google Scholar]
- Sword W, Landy CK, Thabane L, Watt S, Krueger P, Farine D, et al. Is mode of delivery associated with postpartum depression at 6 weeks: a prospective cohort study. BJOG. 2011;118(8):966-77. [PubMed] | [CrossRef] | [Google Scholar]
- Lanes A, Kuk JL, Tamim H. Prevalence and characteristics of postpartum depression symptomatology among Canadian women: a cross-sectional study. BMC Public Health. 2011;11(1):302 [PubMed] | [CrossRef] | [Google Scholar]
- Inandi T, Elci OC, Ozturk A, Egri M, Polat A, Sahin TK, et al. Risk factors for depression in postnatal first year, in eastern Turkey. Int J Epidemiol. 2002;31(6):1201-7. [PubMed] | [CrossRef] | [Google Scholar]
- Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: a study of mothers in Goa, India. Am J Psychiatry. 2002;159(1):43-7. [PubMed] | [CrossRef] | [Google Scholar]
- Xie RH, He G, Liu A, Bradwejn J, Walker M, Wen SW, et al. Fetal gender and postpartum depression in a cohort of Chinese women. Soc Sci Med. 2007;65(4):680-4. [PubMed] | [CrossRef] | [Google Scholar]
- McCabe-Beane JE, Segre LS, Perkhounkova Y, Stuart S, O’Hara MW. The identification of severity ranges for the Edinburgh Postnatal Depression Scale. J Reprod Infant Psychol. 2016;34(3):293-303. [CrossRef] | [Google Scholar]
- Upadhyay RP, Chowdhury R, Salehi A, Sarkar K, Singh SK, Sinha B, et al. Postpartum depression in India: a systematic review and meta-analysis. Bull World Health Organ. 2017;95(10):706-717C. [PubMed] | [CrossRef] | [Google Scholar]
- Ostacoli L, Cosma S, Bevilacqua F, Berchialla P, Bovetti M, Carosso AR, et al. Psychosocial factors associated with postpartum psychological distress during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703 [PubMed] | [CrossRef] | [Google Scholar]
- Figueiredo B, Pacheco A, Costa R. Depression during pregnancy and the postpartum period in adolescent and adult Portuguese mothers. Arch Womens Ment Health. 2007;10(3):103-9. [PubMed] | [CrossRef] | [Google Scholar]
- Klainin P, Arthur DG. Postpartum depression in Asian cultures: a literature review. Int J Nurs Stud. 2009;46(10):1355-73. [PubMed] | [CrossRef] | [Google Scholar]
- Patel HL, Ganjiwale JD, Nimbalkar AS, Vani SN, Vasa R, Nimbalkar SM, et al. Characteristics of postpartum depression in Anand District, Gujarat, India. J Trop Pediatr. 2015;61(5):364-9. [PubMed] | [CrossRef] | [Google Scholar]
- Meky HK, Shaaban MM, Ahmed MR, Mohammed TY. Prevalence of postpartum depression regarding mode of delivery: a cross-sectional study. J Matern Fetal Neonatal Med. 2020;33(19):3300-7. [PubMed] | [CrossRef] | [Google Scholar]
- Pitt B. Atypical depression following childbirth. Br J Psychiatry. 1968;114(516):1325-35. [PubMed] | [CrossRef] | [Google Scholar]
- Martin ME. A maternity hospital study of psychiatric illness associated with childbirth. Ir J Med Sci. 1977;146(8):239-44. [PubMed] | [CrossRef] | [Google Scholar]
- Eckerdal P, Georgakis MK, Kollia N, Wikström AK, Högberg U, Skalkidou A, et al. Delineating the association between mode of delivery and postpartum depression symptoms: a longitudinal study. Acta Obstet Gynecol Scand. 2018;97(3):301-11. [PubMed] | [CrossRef] | [Google Scholar]
- Houston KA, Kaimal AJ, Nakagawa S, Gregorich SE, Yee LM, Kuppermann M, et al. Mode of delivery and postpartum depression: the role of patient preferences. Am J Obstet Gynecol. 2015;212(2):229 [PubMed] | [CrossRef] | [Google Scholar]
- Doi S, Fujiwara T. Combined effect of adverse childhood experiences and young age on self-harm ideation among postpartum women in Japan. J Affect Disord. 2019;253:410-8. [PubMed] | [CrossRef] | [Google Scholar]
- Freitas GV, Cais CF, Stefanello S, Botega NJ. Psychosocial conditions and suicidal behavior in pregnant teenagers: a case control study in Brazil. Eur Child Adolesc Psychiatry. 2008;17(6):336-42. [PubMed] | [CrossRef] | [Google Scholar]
- Siegel RS, Brandon AR. Adolescents, pregnancy, and mental health. J Pediatr Adolesc Gynecol. 2014;27(3):138-50. [PubMed] | [CrossRef] | [Google Scholar]
- Jain A, Tyagi P, Kaur P, Puliyel J, Sreenivas V. Association of birth of girls with postnatal depression and exclusive breastfeeding: an observational study. BMJ Open. 2014;4(6) [PubMed] | [CrossRef] | [Google Scholar]
- de Tychey C, Briançon S, Lighezzolo J, Spitz E, Kabuth B, de Luigi V, et al. Quality of life, postnatal depression and baby gender. J Clin Nurs. 2008;17(3):312-22. [PubMed] | [CrossRef] | [Google Scholar]
- Lagerberg D, Magnusson M. Infant gender and postpartum sadness in the light of region of birth and some other factors: a contribution to the knowledge of postpartum depression. Arch Womens Ment Health. 2012;15(2):121-30. [PubMed] | [CrossRef] | [Google Scholar]
- Kheirabadi G-R. Risk score of postpartum depression (PPD) in rural areas of Isfahan Province, Iran. Iran Arch Iran Med. 2009;12(5):461-7. [PubMed] | [CrossRef] | [Google Scholar]
- Segre LS, O’Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression: the relative significance of three social status indices. Soc Psychiatry Psychiatr Epidemiol. 2007;42(4):316-21. [PubMed] | [CrossRef] | [Google Scholar]
- Ohara MW. Postpartum depression: causes and consequences. 1995 [PubMed] | [CrossRef] | [Google Scholar]
- Kendell RE, McGuire RJ, Connor Y, Cox JL. Mood changes in the first three weeks after childbirth. J Affect Disord. 1981;3(4):317-26. [PubMed] | [CrossRef] | [Google Scholar]
- Hapgood CC, Elkind GS, Wright JJ. Maternity blues: phenomena and relationship to later postpartum depression. Aust N Z J Psychiatry. 1988;22(3):299-306. [PubMed] | [CrossRef] | [Google Scholar]
- Henshaw C. Mood disturbance in the early puerperium: a review. Arch Womens Ment Health. 2003;6(Suppl 2(0)) [PubMed] | [CrossRef] | [Google Scholar]
- Heron J, Craddock N, Jones I. Postnatal euphoria: are “the highs” an indicator of bipolarity? Bipolar Disord. Array. 2005;7(2):103-10. [PubMed] | [CrossRef] | [Google Scholar]
- Reck C, Stehle E, Reinig K, Mundt C. Maternity blues as a predictor of DSM-IV depression and anxiety disorders in the first three months postpartum. J Affect Disord. 2009;113(1-2):77-87. [PubMed] | [CrossRef] | [Google Scholar]
- Manjunath NG, Venkatesh G, Rajanna. Postpartum blue is common in socially and economically insecure mothers. Indian J Community Med. 2011;36(3):231-3. [PubMed] | [CrossRef] | [Google Scholar]
- Stewart DE, Robertson E, Dennis CL, Grace SL, Wallington T. Postpartum depression: literature review of risk factors and interventions. 2003 Available from: http://www.who.int/mental_health/ prevention/suicide/lit_review_postpartum_depression.pdf
[PubMed] | [CrossRef] | [Google Scholar]